One of the keys to a better version of you, mentally and physically, is sleeping well. We want all of our industry members to sleep as well as they can that’s why EIC have partnered with Sleepstation. Sleepstation is a clinically validated sleep improvement programme that can help you learn how to control and optimise your sleep to get the best sleep possible. Designed by experts and backed by science, the online service is proven to combat even the most severe insomnia. Their team will help you identify the underlying causes of your sleep problem and provide the personal support and guidance needed to improve your sleep. Sleepstation delivers remote care with a personal touch and that's what makes it so effective. Therapeutic support through Sleepstation is available to those in need and meeting our charity eligibility criteria.

This month we focus on the important topic of Men’s Health. This is particularly important for our industry as 85% of the employees are men. Globally, men die on average six years earlier than women, and for reasons that are largely preventable. It doesn’t have to be that way; we can all take action to live healthier, happier and longer lives. Generally, men are more reluctant to visit medical centres and or doctors and studies have proven women are 100% more likely to visit the doctors. Sometimes masculinity can drive riskier behaviour such as dangerous driving and going that little bit further can have repercussions on our health. We explore the most prevalent male cancers, men's mental health and common health issues men face within the industry.

This month is all about men’s health and what a better way to show that you care than joining in with a challenge with your colleagues or friends.
Why?
Globally, men die on average six years earlier than women, and for reasons that are largely preventable. It doesn’t have to be that way; we can all take action to live healthier, happier and longer lives and promote this within our communities. Our industry consists of 85% male, so it is very important to raise awareness about men’s physical and mental health in our sector
How?
- Grow a moustache for 30 days in November and raise awareness on men’s health in our sector.
- Feeling adventurous? Why don’t you host a charity head shave and shave it ALL off at the end of the month? This could raise much needed funds for electrical industry. Get in touch with us and we can help you get this off the ground. Contact: This email address is being protected from spambots. You need JavaScript enabled to view it.
- Post the above image and text below on your social media channels and tag @electricalcharity #EIC
I am taking part in menmeetmoustache this month with EIC and will grow my moustache for 30 days! Look out for my before and after pictures at the end of the month. Join in with me, raise awareness and vital funds for our industry: https://bit.ly/3BVxtCo @electricalcharity - Post your progress pictures and donate to our fundraising page if you can: https://bit.ly/3DQkHpn

In the UK, the male suicide rate is its lowest since 1981 – 15.5 deaths per 100,000. But suicide is still the single biggest killer of men under the age of 45. And a marked gender split remains. For UK women, the rate is a third of men’s: 4.9 suicides per 100,000. It’s the same in many other countries. Compared to women, men are three times more likely to die by suicide in Australia, 3.5 times more likely in the US and more than four times more likely in Russia and Argentina. WHO’s data show that nearly 40% of countries have more than 15 suicide deaths per 100,000 men; only 1.5% show a rate that high for women. Suicide is a hugely sensitive, complex issue with a tangled multitude of causes – and the very nature of a death by suicide means we can never fully know the reasons behind it. Still, as mental health awareness has grown, there is greater public understanding about potential contributing factors. One of the questions that has persisted, though, regards the gender gap.
Risk Factors
One key element in this gender gap is communication. It’s too simplistic to say women are willing to share their problems and men tend to bottle them up. But it is true that, for generations, many societies have encouraged men to be “strong” and not admit they’re struggling. It often starts in childhood. The society is programmed to tell boys that 'boys don't cry'. We condition boys from a very young age to not express emotion, because to express emotion is to be 'weak'. Men may be less likely to admit when they feel vulnerable, whether to themselves, friends, or a GP. They also can be more reticent than women to see a doctor. A UK British Medical Journal study found general primary care consultation rates were 32% lower in men than women. (Consultation rates for depression, assessed by whether patients received antidepressant prescriptions, were 8% lower in men than women).
Men seek help for mental health less often. It's not that men don't have the same issues as women – but they're a little less likely to know they have whatever stresses or mental health conditions that are putting them at greater risk for suicide. Other risk factors can be related to family or work. When there's an economic downturn that results in increased unemployment, for example, there tends to be an associated increase in suicide – typically 18-24 months after the downturn. One 2015 study found that for every 1% increase in unemployment there is a 0.79% increase in the suicide rate. Read more
Here are our top 5 things to know and do:
- Spend time with people who make you feel good. Stay connected. Your mates are important and spending time with them is good for you. Catch up regularly, check in and make time.
- Talk, more. You don’t need to be an expert and you don’t have to be the sole solution, but being there for someone, listening and giving your time can be lifesaving.
- Know the numbers. At 50, talk to your doctor about prostate cancer and whether it’s right for you to have a PSA test. If you are black or have a father or brother with prostate cancer, you should be having this conversation at 45. Know your numbers, know your risk, talk to your doctor.
- Know thy nuts. Simple. Get to know what’s normal for your testicles. Give them a check regularly and go to the doctor if something doesn’t feel right.
- Move, more. Add more activity to your day. Do more of what make you feel good.

- Take a walking meeting
- Park further away from the station
- Get off the bus a stop or two earlier
- Instead of the lift, take the stairs
- Cycle to work instead of driving

It is important to talk about our mental health. This men’s month the Electrical Industries Charity want to highlight the free and confidential support available to the industry of which 85% is men. Changes in our work and personal life can be stressful even if they are typically things which are and should be celebrated like a new baby, wedding, or a promotion. Nick, a wholesale employee of three years, was recently promoted to manage a team within his workplace. Nick contacted the Electrical Industries Charity using the online support form as he began to feel insecure in his new role.
Beginning a new role internally or externally to your company can be stressful. Nick felt a huge amount of pressure stepping into the role, especially as the person he was replacing was well respected by both colleagues and customers. Stress can cause anxiety and sleep deprivation and Nick was suffering from both. When speaking to the Electrical Industries Charity welfare team Nick spoke of imposter syndrome. Imposter syndrome refers to when a person feels like a fraud despite their evidence of success and competency. The Charity welfare team discussed with Nick the root of his feelings and Nick described he has not felt so anxious or stressed since school. Nick disclosed he had been bullied during school and he had found his teenage years difficult. Nick had struggled with self-esteem issues and anxiety and these feelings were creeping back since beginning his new role.
1 in 3 of all Electrical Industries Charity cases involve mental health and 76% of those involve anxiety and/or depression. The Charity award hundreds of thousands of pounds of grants to those struggling with their mental health every year and can source and fund therapy sessions for sector colleagues in need. The Charity organised Cognitive Behavioural Therapy (CBT) sessions for Nick which would help him engage with past experiences to support him through his current anxiety. CBT works by rewiring thought processes to help develop positive thought patterns and dissemble disruptive thinking leading to positive behaviours and emotions. Nick committed to six CBT sessions all funded through the Charity’s Employee and Family Programme which gives employees of the electrical and energy sector free and confidential support.
Nick completed his therapy sessions after work and found with each session he had a renewed confidence in his abilities. Nick is now thriving within the workplace and has developed a productive and positive relationship with his team. Since completing therapy Nick has overcome his imposter syndrome and feels well respected; he is hoping for more promotion and praise in the future. The Electrical Industries Charity is here to support you and help you to thrive in our industry. If you need assistance, please contact This email address is being protected from spambots. You need JavaScript enabled to view it. or 0800 652 1618.


November is men’s month and this year the Electrical Industries Charity is highlighting testicular cancer and how important it is to be in the know about testicular cancer. Testicular cancer is mostly diagnosed in young men and men who have undescended testes at birth or have a family history of testicular cancer are most at risk. Cancer is daunting and being diagnosed with testicular cancer can be incredibly scary. James, a power station worker of 4 years, was diagnosed with testicular cancer at just 27. James contacted the charity via the helpline after being diagnosed with stage 1 testicular cancer three weeks earlier. James had always been incredibly active and was in shock he had developed cancer at such a young age. James had managed to catch his cancer early and was advised his cancer had not spread – a positive sign but the first treatment option was to remove his right testicle. Understandably, James was distraught at the prospect of surgery and was struggling to cope with the impact surgery may have. James believed post operation he would be less of a man and unable to have children. James and his fiancée had always wanted a family and he feared he would be left infertile and their relationship irrevocably damaged. James had not spoken to his doctor, his partner or family about his concerns and instead had let them bottle up inside of him – he was riddled with anxiety and stress and was increasingly tearful.
The Electrical Industries Charity encouraged James to speak to his doctor to understand the likelihood of infertility and impotence. James had done his own research but found himself overwhelmed whenever he read about testicular cancer. The Charity welfare team understood James’ fear but told him knowledge is power. Although there may be a chance of infertility or impotence the doctor is the best person to advise and help him understand further treatment options. James was also anxious to speak to his fiancée, he feared rejection should he be infertile and felt his place as the protector and solid support structure would be destroyed. The charity team also funded counselling sessions to give James a safe non-judgemental outlet while he was struggling to speak to his partner and his family. Through counselling James worked through his grief and anxiety and after two sessions he opened up to his fiancée. James’ fiancée reassured him they were a team, and they will remain a team to find the best support possible. James’ partner then attended the doctor’s appointment with him to establish the likelihood of infertility, impotence and return of cancer.
James’ doctor advised that by removing James’ right testicle his chances at making a full recovery are greatly improved and his sex life and fertility should not be affected. About 1 in 50 will get new testicular cancer in their remaining testicle but in such circumstances, there is the opportunity to only remove part of the testicle. With James’ fears eased and his fiancée’s support James underwent surgery and a single dose of chemotherapy to eradicate the cancer. Post operation James attended two more charity funded counselling sessions and felt equipped to face life post cancer with the support of his fiancée. Since James’ doctor has confirmed the cancer was successfully eradicated and he is now having bi-yearly follow up appointments. James and his fiancée married in the Summer and are now thinking about adding to their family. The Charity continue to check in on James and should he need further support the Charity would be more than happy to help.
It is so important to check your testicles and know how they should feel. If you spot anything unusual, please seek medical advice. The Electrical Industries Charity are here to help you through any stage of your diagnosis. Please contact the welfare team on This email address is being protected from spambots. You need JavaScript enabled to view it. or call 0800 652 1618.

Prostate cancer is the most diagnosed cancer in men in the UK. Know the facts and act early.
Early detection is key:
The difference between early detection and late detection can be life and death.
Who's at risk?
Your risk of developing prostate cancer increases with age, but that doesn’t mean it’s a disease that only affects old men. Prostate cancer is the second most common cancer in men worldwide. Men who are black, and men who have a family history (a brother or father with prostate cancer), are 2.5x more likely to get prostate cancer.
If you’re 50, you should be talking to your doctor about PSA testing. If you’re black, you need to start that conversation at 45. And if you have a brother or father with prostate cancer in their history, do it at 45.
What's a PSA test?
It’s a simple routine blood test that is used to determine the measurement of Prostate Specific Antigen (PSA) concentration in the blood, it is the primary method of testing for prostate cancer. You should be talking to your doctor about whether testing is right for you.
So, what do you need to do?
Go to the doctor and ask about PSA testing. Catch prostate cancer early!

Only men have a prostate gland. The prostate gland is usually the size and shape of a walnut and grows bigger as you get older. It sits underneath the bladder and surrounds the urethra, which is the tube men urinate and ejaculate through. Its main job is to help make semen – the fluid that carries sperm. Prostate cancer occurs when some of the cells in the prostate reproduce far more rapidly than normal, resulting in a tumour. Prostate cancer often grows slowly to start with and may never cause any problems. But some men have prostate cancer that is more likely to spread. These prostate cancer cells, if left untreated, may spread from the prostate, and invade distant parts of the body, particularly the lymph nodes and bones, producing secondary tumours in a process known as metastasis.
Detecting prostate cancer:
Not everyone experiences symptoms of prostate cancer. Many times, signs of prostate cancer are first detected by a doctor during a routine check-up. Some men, however, will experience changes in urinary or sexual function that might indicate the presence of prostate cancer.
Signs and symptoms:
• A need to urinate frequently, especially at night
• Difficulty starting urination or holding back urine
• Weak or interrupted flow of urine
• Painful or burning urination
• Difficulty in having an erection
• Painful ejaculation
• Blood in urine or semen
• Frequent pain or stiffness in the lower back, hips, or upper thighs
Treating prostate cancer:
Treatment options are many and varied. Testing still can’t answer lots of key questions about disease aggression, prognosis and progression. If you have been diagnosed with prostate cancer, it's important to keep in mind that many prostate cancers are slow growing and may not need surgery or other radical treatment.
Treatment options include:
• Active Surveillance
• Prostatectomy
• Radiotherapy
• Hormone Therapy
• Chemotherapy
If you experience any symptoms or are over the age of 45 speak to your GP today! If you are living with prostate cancer and looking for advice and support reach out to Prostate Cancer UK. They provide a range of information and support so you can choose the services that work for you. All their services are open to men, their family, and their friends.

In United Kingdom, testicular cancer is the most commonly diagnosed cancer in young men.
Who's at risk?
In United Kingdom, testicular cancer is the most diagnosed cancer in young men. Men with undescended testes at birth, or who have a family history, like a father or brother who has had testicular cancer, are at an increased risk. And if you’ve had testicular cancer before, there’s also a heightened risk it could return.
The facts about testicular cancer:
Testicles are responsible for the production of male hormones (mostly testosterone) and sperm. Testicular cancer starts as an abnormal growth or tumour that develops in one or both testicles. There are several types of testicular cancer, but the most common is the germ cell tumour.
If you've been diagnosed with testicular cancer:
The most important step is to talk to your doctor about treatment choices. You may consider getting a second or third doctor’s opinion.
Hear from Mo Bro Ben Bowers about his experience with his testicular cancer.
Treatment options:
Testicular cancer is a highly treatable cancer and can be effectively treated, and often cured, if diagnosed and treated early. Advanced testicular cancer can also be cured with treatment including:
- Orchiectomy (surgical removal of the affected testis), done under general anaesthetic
- Chemotherapy or radiotherapy, often prescribed after surgery to treat any remaining cancer cells that may have spread to other parts of the body, such as lymph nodes
Side effects:
Testicular cancer and the removal of one testicle should not alter your ability to have sex or have children. The effect on fertility following removal of one of the testicles is minimal as a single testicle produces such large numbers of sperm. Men with testicular cancer should talk to their oncologist about sperm banking before commencing chemotherapy or radiation therapy.
So, know your nuts - it's that simple!
The best thing you can do for your testicles is give them a bit of a feel each month or so, and if something doesn’t seem right, head to the doctor. If you notice a change in size or shape, a lump that wasn’t there before, or if they become painful to touch, see a doctor. Don’t panic but do get it checked out.
Here is a guide to checking your testicles.

Men are more likely than women to drink excessively. Excessive drinking is associated with significant increases in short-term risks to health and safety, and the risk increases as the amount of drinking increases. Men are also more likely than women to take other risks (e.g., drive fast or without a safety belt), when combined with excessive drinking, further increasing their risk of injury or death.
Drinking levels among men
• Approximately 58% of adult men report drinking alcohol in the last 30 days
• Approximately 23% of adult men report binge drinking 5 times a month, averaging 8 drinks per binge
• Men are almost two times more likely to binge drink than women
• Most (90%) people who binge drink are not alcoholics or alcohol dependent
• About 4.5% of men and 2.5% of women met the diagnostic criteria for alcohol dependence in the past year

Injuries and deaths because of excessive alcohol use
• Men consistently have higher rates of alcohol-related deaths and hospitalizations than women.
• Among drivers in fatal motor-vehicle traffic crashes, men are almost twice as likely as women to have been intoxicated
(i.e., a blood alcohol concentration of 0.08% or greater).
• Excessive alcohol consumption increases aggression and, as a result, can increase the risk of physically assaulting another person.
• Men are more likely than women to commit suicide, and more likely to have been drinking prior to committing suicide.
Reproductive Health and Sexual Function
Excessive alcohol use can interfere with testicular function and male hormone production resulting in impotence, infertility, and reduction of male secondary sex characteristics such as facial and chest hair. Excessive alcohol use is commonly involved in sexual assault. Also, alcohol use by men increases the chances of engaging in risky sexual activity including unprotected sex, sex with multiple partners, or sex with a partner at risk for sexually transmitted diseases.
Cancer
Alcohol consumption increases the risk of cancer of the mouth, throat, esophagus, liver, and colon in men.

Alcohol dependence, sometimes known as ‘alcoholism’, is the most serious form of drinking problem and describes a strong, often uncontrollable, desire to drink. Drinking plays an important part in the day to day life of alcohol dependent people, which could lead to building up a physical tolerance or experiencing withdrawal symptoms if they stop.
There are varying degrees of alcohol dependence and they don’t always involve excessive levels of drinking. If you find that you ‘need’ to share a bottle of wine with your partner most nights of the week, or always go for a few pints after work, just to unwind, you’re likely to be drinking at a level that could affect your long-term health. You could also be becoming dependent on alcohol. If you find it very difficult to enjoy yourself or relax without having a drink, you could have become psychologically dependent on alcohol. Physical dependence can follow too, that is your body shows withdrawal symptoms, such as sweating, shaking and nausea, when your blood alcohol level falls.
Alcohol dependence can contribute to mental health problems
Anxiety, depression and suicidal feelings can all develop when you’re alcohol dependent. This is because regular, heavy drinking interferes with neurotransmitters in our brains that are needed for good mental health. Being dependent on alcohol can affect your relationships with your partner, family, and friends. It might mean you don’t perform so well at work and if that continues for any length of time you could face losing your job, leading to financial problems as well. These issues can also contribute to depression and anxiety. Alcohol can also make you more aggressive. If you use alcohol to try and improve your mood, you may be starting a vicious cycle.
If you think your mental health is suffering because of your drinking, but you feel you’re not able to stop, ask for professional help. Start with a visit to your GP or by contacting one of the organisations listed at the end of this page. Alcohol can even make you more aggressive.
How to reduce your risk of becoming alcohol dependent
Taking regular breaks from alcohol is the best way to lower your risk of becoming dependent on it. If you drink regularly, your body builds up a tolerance to alcohol. Tolerance is a physiological response we have to any drug: the more you consume, the more your body needs to have the same effect. Regular drinking induces certain enzymes in your liver that break up (metabolise) alcohol. If you drink heavily over weeks or months, levels of these enzymes go up, your tolerance builds, and you need more alcohol to get the same effects.
Brain systems get tolerant to alcohol too, and although you may be able to walk a straight line after drinking quite a lot, this means the brain has adapted so that next day the brain cells ‘expect’ alcohol. Withdrawal symptoms such as anxiety and jitteriness occur, and you can find yourself drinking alcohol just to relieve that. When you’re drinking most days, you can become psychologically dependent on alcohol too. Breaking your drinking cycle is an important way to test for – and tackle – this kind of dependence. It can prevent your body from becoming accustomed to alcohol and help to lower or ‘reset’ your tolerance.
Staying in control
Drinking within the low risk unit guidelines will help you keep your drinking under control. Here are three ways you can cut back: Try alternative ways to deal with stress other than alcohol. Instead of reaching for a beer or glass of wine after a hard day, go for a run, swim or to a yoga class, or a talk to a friend about what’s worrying you.
Keep track of what you’re drinking. Your liver can't tell you if you're drinking too much, but MyDrinkaware can. It can even help you cut down.
Give alcohol-free days ago. If you drink regularly, your body starts to build up a tolerance to alcohol. This is one of the main reasons why many medical experts recommend taking regular days off from drinking to ensure you don't become addicted to alcohol. Test out having a break for yourself and see what positive results you notice.

Further information
Your GP can help you figure out if you should make any changes in your drinking and offer help and advice along the way.
If you’re concerned about someone’s drinking, or your own, Drinkline runs a free, confidential helpline. Call 0300 123 1110.
Alcoholics Anonymous: If you need help with a drinking problem you can phone the national helpline on 0800 9177650 or email:
This email address is being protected from spambots. You need JavaScript enabled to view it.
Addaction: For all general enquiries and concerns, you can email Addaction on This email address is being protected from spambots. You need JavaScript enabled to view it. . To find your nearest service in England or Scotland, visit the Service Finder” section of the website www.addaction.org.uk

Causes of colour blindness:
Colour blindness is a usually a genetic (hereditary) condition (you are born with it). Red/green and blue colour blindness is usually passed down from your parents. The gene which is responsible for the condition is carried on the X chromosome and this is the reason why many more men are affected than women.
8% of the male population and 4.5% of the population of the UK are colour blind and there are estimated to be over 250 million colour blind people worldwide. Many people with a colour vision deficiency have inherited their condition from their mother, who is normally a ‘carrier’ but not colour blind herself. Some people also acquire the condition because of long-standing diseases such as diabetes, multiple sclerosis, some liver diseases and almost all eye diseases. The effects of colour vision deficiency can be mild, moderate, or severe depending upon the defect. If you have inherited colour blindness your condition will stay the same throughout your life – it won’t get any better or worse.
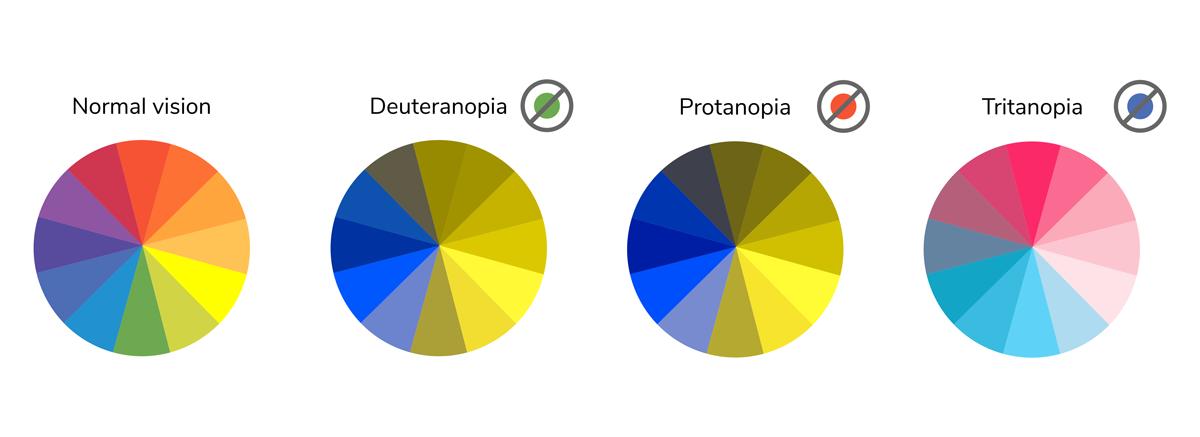
The retina of the eye has two types of light-sensitive cells called rods and cones. Both are found in the retina which is the layer at the back of your eye which processes images. Rods work in low light conditions to help night vision, but cones work in daylight and are responsible for colour discrimination. There are three types of cone cells and each type has a different sensitivity to light wavelengths. One type of cone perceives blue light, another perceives green and the third perceives red. When you look at an object, light enters your eye and stimulates the cone cells. Your brain then interprets the signals from the cones cells so that you can see the colour of the object. The red, green, and blue cones all work together allowing you to see the whole spectrum of colours. For example, when the red and blue cones are simulated in a certain way you will see the colour purple. The exact physical causes of colour blindness are still being researched but it is believed that colour blindness is usually caused by faulty cones but sometimes by a fault in the pathway from the cone to the brain.
People with normal colour vision have all three types of cone/pathway working correctly but colour blindness occurs when one or more of the cone types are faulty. For example, if the red cone is faulty you won’t be able to see colours containing red clearly. Most people with colour blindness can’t distinguish certain shades of red and green.

Colour blind people face many difficulties in everyday life which normally sighted people just aren’t aware of. Problems can arise in even the simplest of activities including choosing and preparing food, gardening, sport, driving a car and selecting which clothes to wear. Colour blind people can also find themselves in trouble because they haven’t been able to pick up a change in someone’s mood by a change in colour of their face, or not noticed their child getting sunburnt.
Colour blindness can affect access to education, exam grades and career choice.
Here are a just a few examples of typical, everyday problems:
- Most red/green colour-blind people won’t know if they’ve cooked a piece of meat rare or well done and they’re unlikely to be able to tell the difference between green and ripe tomatoes or between ketchup and chocolate sauce.
- Colour blind people often try to eat unripe bananas because they can’t tell the difference between a green unripe banana and a yellow ripe banana – to them because both of the colours are the same shade they often think they are the same colour.
In the UK society doesn’t generally think of colour blindness as a disability, but in most cases colour blindness should be considered to be a disability and therefore employers, schools and businesses must treat colour blindness in the same way they would any other disability. Unfortunately, the Guidance Notes to the Equality Act 2010 are misleading but the Government Equalities Office recognises colour blindness can be a disability, despite this ambiguity.
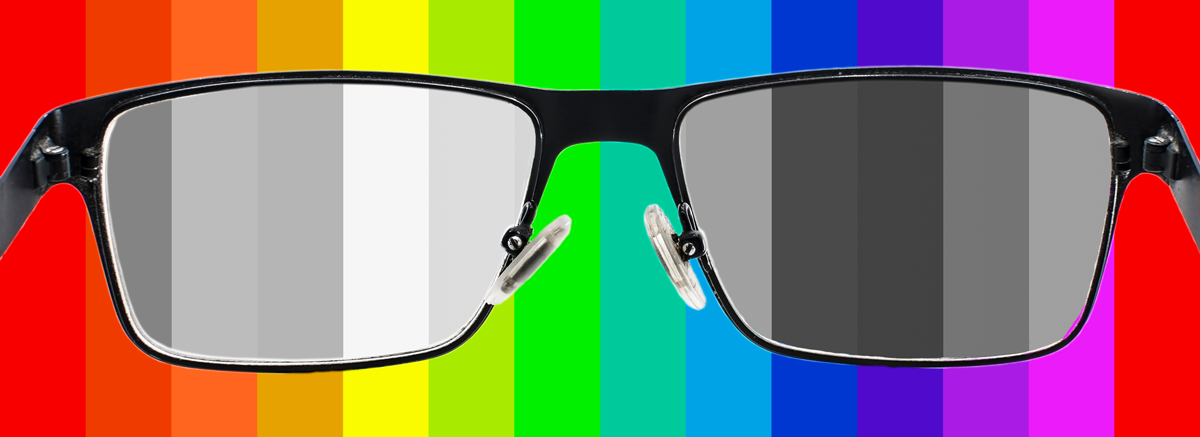
Treatment:
There is currently no treatment for inherited colour blindness. Some colour-blind people have found some coloured filters and some lenses might help them to distinguish between some colour combinations in certain situations, whilst others report no effect or that they can cause further confusion. There is hope on the horizon for a ‘cure’ for inherited colour vision deficiency using gene technology – for more information visit www.neitzvision.com. This will involve injecting genetic material into the eye so is not for the faint-hearted! Now there have been no trials on humans yet. For acquired colour vision deficiency, once the cause has been established and treated, your vision may return to normal.

Statistics: Noise Exposure and Hearing Protection
- About 51% of all workers in Construction have been exposed to hazardous noise.
- 31% of noise-exposed Construction workers report not wearing hearing protection.
Statistics: Hearing Loss and Tinnitus
- Approximately 14% of all Construction workers have hearing difficulty.
- About 7% of all Construction workers have tinnitus.
- About 25% of noise-exposed tested Construction workers have a material hearing impairment. Hearing impairment is hearing loss that impacts day-to-day activities.
- 16% of noise-exposed tested Construction workers have hearing impairment in both ears.
Noise Hazards in Construction
A construction site is a noisy place to work no matter what precautions are taken. Regular 8-hour exposures to 85 dBA can damage your hearing. If you have to use a jackhammer for 1 hour per day, you may experience hearing damage. The higher the noise level, the faster the hearing loss. This is bad news for construction workers because much of the equipment they use regularly is above the 85 dBA exposure level:
• Jackhammer: 100 dBA
• Chop saw: 105 dBA
• Chain saw: 110 dBA
• Hammer drill: 115 dBA

The National Institute for Occupational Safety and Health (NIOSH) found that a 25-year old carpenter is likely to have the ears of 50-year old person who has not been exposed to noise. You may be exposed to various types and levels of noise of varying duration for much of your workday. But hearing damage, and the symptoms, can take time to develop. That’s why employers should provide yearly hearing tests for workers routinely exposed to hazardous noise levels. This can help determine if more needs to be done to protect your hearing. There are several devices, like sound meters and dosimeters, that measure noise levels, but you often don’t have access to them while you’re working. So what do you do? Use the 2-to-3 foot rule: Standing an arm’s length away from a co-worker (i.e. 2 to 3 feet), if you need to raise your voice to be heard, then the sound level is probably at or above 85 dBA.
Tell Tale Signs of Hearing Loss
Most occupational hearing loss is gradual, though the rate is greatest during the first 10 years of exposure. Continued noise exposure can cause hearing loss of frequencies needed to hear speech.
Awareness of the symptoms can help you identify possible damage and take the precautions necessary to reduce the damage. Signs of hearing loss include:
- Noise or ringing in your ears
- Difficulty hearing people on the phone
- Regular speech sounds like mumbling
- Difficulty hearing people when there’s background noise
- Trouble hearing cell phone rings or back-up alarms
- People must repeat what they said
- You hear muffled or distorted speech sounds
Also, OSHA recommends a self-test for workers who drive to work. Before you get out of your vehicle, turn off the engine and set the radio to a talk radio station so it’s barely loud enough to hear. At the end of your workday before you start the engine, note whether you can hear the radio with the power on. If you have trouble hearing it, there may be damage and you’ll need to better protect against high noise levels.
Protecting Yourself
Sometimes administrative and engineering controls aren’t enough to adequately reduce noise to safe levels. Construction workers likely to be exposed to harmful noise should wear hearing protective devices. The various types of protection available are designed for specific conditions. Proper and consistent use of these devices is imperative for effective protection. If they aren’t comfortable and convenient, you might not use them, so it’s important that employers procure well-fitting, easy-to-use PPE.
When selecting and wearing hearing PPE, consider:
• Communication needs
• Convenience and comfort
• Noise level of the task
• Noise reduction of the devices
• Hearing ability
• Hygiene
Typical hearing protective devices include roll down foam plugs, reusable earplugs, custom moulded plugs, canal caps, and earmuffs.
Remember: Your employer is required to provide you with the necessary PPE. If you don’t see it, ask for it. More info