The charity is adapting its support service to help industry members through this pandemic. We are providing regular updates for the industry and offering lots of useful information, advice and support links on issues that may be affecting you or your family members during COVID-19 such as:
Practical Support - Reducing personal debt, helpful advice for those who are worried about their and the person that they care for safety - Salary and more.
Employed and Self-employed support - Help and Guidance for employers who are looking to furlough employees or struggling with Covid-19 generally and more.
Mental Health support - Feeling the pressure to be productive? A useful toolkit to support your mental health during the pandemic, how to protect your mental health during the pandemic and more.
Housing support - The welfare team are supporting renters who need to write to their landlords in support for rent holidays and more.
Welfare benefit Support - If you are self-employed or lost your job because of COVID-19 consider applying for universal credit? And more.
Legal support – Advice for employees requiring legal support during the pandemic and more.
Self-Isolation - Guide for social distancing and more.
For all this information and more please visit our COVID-19 regular updates website page at the link below:


Feeling overwhelmed or overloaded? Find yourself in a carers position for elderly parents, a sick child or partner perhaps? Looking after yourself, is just as important as looking after others and we can help support with the added responsibilities, emotional side and having that extra weight on your shoulders too. Have a look at the items we cover off this month.

What counts as supporting or caring for someone else?
Supporting someone else is sometimes called caring. You are a carer if you provide (unpaid) support and care for someone who has an illness, disability, mental health problem or addiction. People often assume that carers tend to be women, but research shows that around four in ten carers are men.
Being someone’s carer probably only describes part of your relationship with them. You may also be a parent, partner, sister, brother, child, friend or other family member. This relationship can be just as (or more) important to you. You may also have other caring roles as well, for example as a parent to other children.
Supporting others can be mentally and physically exhausting. The time you spend caring can really vary too – some people look after someone for just a short time and others find themselves caring for someone for the long term.

Caring and the benefits system
The benefits system only defines you as a carer if you meet the criteria for Carers Allowance (the main welfare benefit for carers in the UK).
But even if you don't meet this criteria, you may still be considered a carer by your local authority (council) and have needs for additional support. See our legal page on carers' social care rights for more information.
What might I have to do if I am caring for or supporting someone else?
Caring can mean a range of things. Being patient and giving can feel like part of the normal give and take of any relationship, but sometimes you might find yourself spending a lot more time and effort helping someone else.
You may provide a range of support including:
• giving emotional support
• helping someone seek help for a mental health problem
• helping someone cope with a mental health problem
• cooking and cleaning
• personal care like washing and going to the toilet
• budgeting and looking after finances
• supporting them to live with others in your family (e.g. brothers and sisters)
• helping other family members understand the needs of the person you are caring for
• giving medicine or providing medical care
• going to appointments and advocating on their behalf (helping them express their views and wishes)
• checking they are safe.
Sometimes they may not accept they need care or support from you. This can make things extra hard. Have a look at our info on what to do when they won't get help or they push you away and say things that upset you.
"I was completely unaware that what I was doing was a carer role and the effect it was having on me. I didn't think about reaching out for support myself."

It’s normal for children to occasionally forget their homework, daydream during class, act without thinking, or get fidgety at the dinner table. But inattention, impulsivity, and hyperactivity are also signs of attention deficit hyperactivity disorder (ADHD), sometimes known as attention deficit disorder or ADD.
ADHD is a common neurodevelopmental disorder that typically appears in early childhood, usually before the age of seven. ADHD makes it difficult for children to inhibit their spontaneous responses—responses that can involve everything from movement, to speech, to attentiveness. We all know kids who can’t sit still, who never seem to listen, who don’t follow instructions no matter how clearly you present them, or who blurt out inappropriate comments at inappropriate times. Sometimes these children are labelled as troublemakers or criticized for being lazy and undisciplined. However, they may have ADHD
If your child needed help – naturally you would do whatever you could to support them. But sometimes, circumstances are out of your control. That’s why the Electrical Industries Charity (EIC) is here to help take the strain off families facing challenging times. This is achieved through their Employee and Family Support Programme (EFP) which is part of the Employee Assistance Programme (EAP).
A good example of one of the many families EIC has helped is Martin and Carol and their daughter Katie.

Carol first contacted the EIC for support when Katie started attending primary school, as Katie’s teachers began to recognise that she may have learning difficulties and she was also displaying signs of ADHD (Attention Deficit Hyperactivity Disorder). Katie was really struggling, predominantly with restlessness, retaining information and maintaining focus, often flitting between tasks with an inability to remain on the same activity for a prolonged period. Carol explained that Katie was also finding general organisation quite challenging, resulting in her often misplacing her belongings. Her teachers had also expressed concerns that Katie would often daydream and required a member of staff to keep her on task. Her academic ability was reported to be below the expected level for her age.
It can be difficult to distinguish between ADHD and normal “kid behaviour.” If you spot just a few signs, or the symptoms appear only in some situations, it’s probably not ADHD. On the other hand, if your child shows a number of ADHD signs and symptoms that are present across all situations—at home, at school, and at play—it’s time to take a closer look.
Katie’s combination of symptoms were causing her to feel distressed and unhappy. Katie also had a diagnosis of dyslexia which may have accounted for her struggles with organisation and retention of information, but Carol was keen to investigate the suggestion from her teachers that there may be underlying ADHD.
Statistically, across Europe, boys are five times more likely to have ADHD in comparison to girls and in the UK, this rises to six times more likely. Unless girls display obvious symptoms, such as disruptive behaviour or hyperactivity, they are less likely to be recognised as potentially requiring an ADHD screening and are therefore often left unsupported or labelled as ‘day-dreamers’ and causing them to slip under the radar.
Katie had been referred through the NHS for an ADHD assessment, however the wait for this process was 12 months. Martin and Carol were concerned for katies mental health and wellbeing and her falling further behind academically. Without a formal diagnosis Katie was unable to apply or receive further support. The diagnosis would hopefully qualify the family to obtain an Educational Health Care Plan (EHCP), which would provide them access to the funding required for the additional support in the classroom.
To fast-track this process, the EIC arranged for a private ADHD assessment to be carried out within 6 weeks, which enabled a specialist psychologist to observe Katie at school and to speak with her teachers to gain an insight into how she was coping in a classroom environment. Martin and Carol also filled in detailed questionnaires which were analysed by a clinician before a formal assessment was carried out by a Child and Adolescent Psychiatrist at the clinic.
A formal diagnosis of ADHD was finally made by the Psychiatrist and Katie’s parents received a full written report, medication recommendations and strategies which would benefit Katie and ease her daily routine.
Life with a child or teen with attention deficit hyperactivity disorder (ADHD or ADD) can be frustrating, even overwhelming. But as a parent you can help your child overcome daily challenges, channel their energy into positive arenas, and bring greater calm to your family. And the earlier and more consistently you address your child’s problems, the greater chance they have for success in life.
Katie is responding well to the medication and is coping much better in a classroom environment. She has begun to join in with classroom-based activities and is able to maintain her focus for a longer period. Carol and Martin are now in the process of applying for an EHCP.
Thanks to support from the industry, every year the Electrical Industries Charity is able to offer hundreds of our industry colleagues both practical and emotional support during their time of need.
If you or someone you know is struggling and requires support, please contact the EIC support team: This email address is being protected from spambots. You need JavaScript enabled to view it.
or 0800 652 1618.

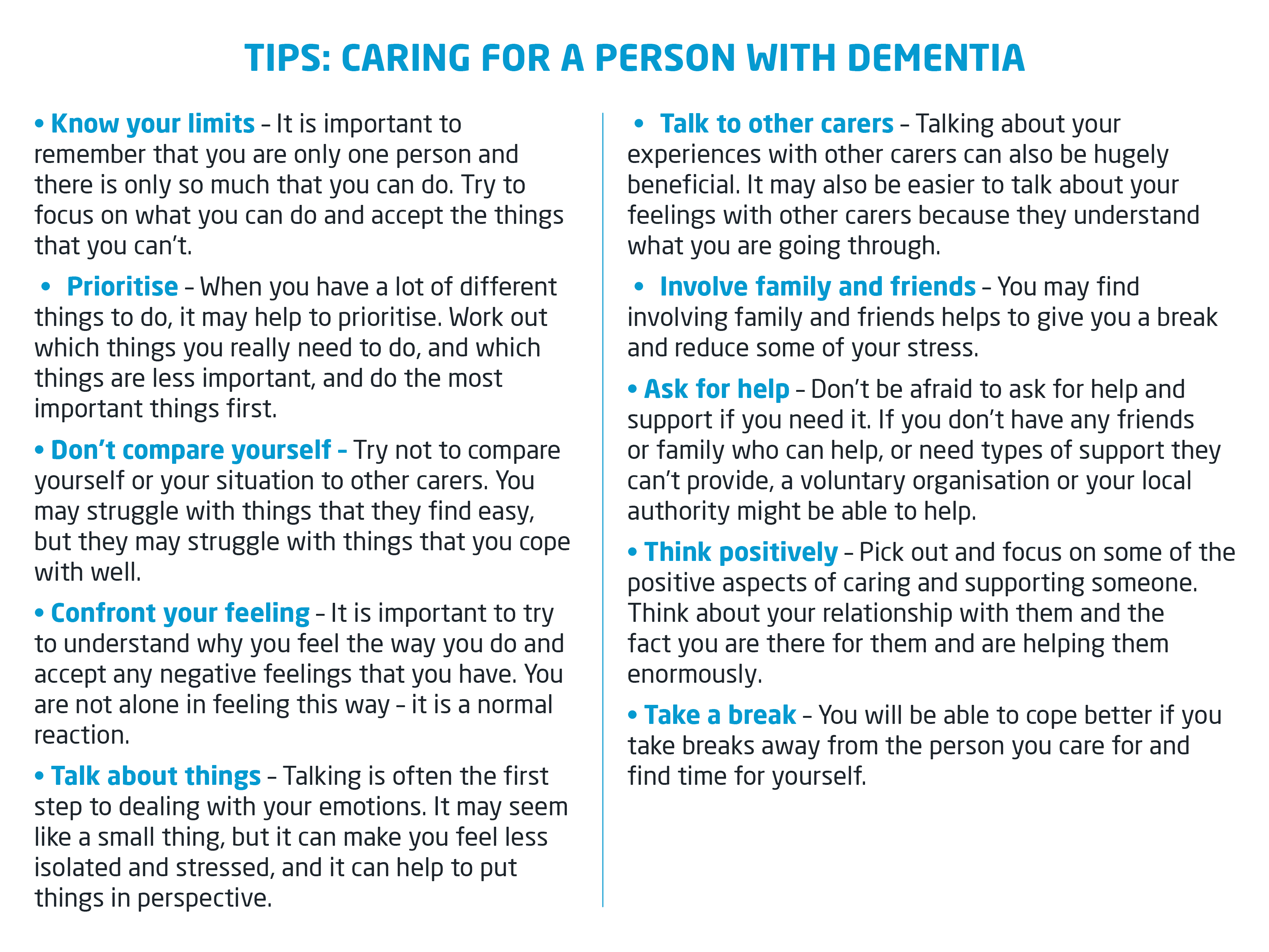
As a carer you spend a lot of your time focusing on someone else. You may feel as if you just have no time at all for yourself. But looking after your own wellbeing is important for you and for them. Below are some suggestions that others have said they find helpful. Even just choosing one small thing to change might help you feel more able to cope.
Talk about how you feel
It can be really important to have someone to talk to, especially if you are struggling to cope. You could:
• share your feelings with someone you trust – this might be a family member or a friend
• join a support group for carers
• contact the Carers UK helpline

Ask for help if you need it
Most carers need some additional support. Think about whether family and friends could help you. People don't always know what they can do to help but may be happy to lend a hand if you can tell them what you need.
Be realistic
If you take on too much, you may feel as if you never achieve anything. If you have a clear idea about what you can do and accept the parts that you can't change or do alone, you may feel more able to cope.
You could try to:
• make a list of all the support the person you are caring for needs
• identify (with them if possible) what you can do and what you need help with
• think about how you'll be able to tell when you need a break and write this down too.
Stay organised
Staying organised can help you feel more in control. You could keep a schedule or planner of your daily routine and make sure that you keep all important information and medication in one place. But don't beat yourself up if you get muddled or things get lost. You've got a lot to think about.
Support their independence
Work with them to see how they can help themselves and work out what support they need from you and whether there are times that they can cope on their own. It's important to help them have some control over their care. You may find this means taking a step back or supporting decisions that are not what you would do. But it can also mean that you are able to find a balance in your relationship and perhaps a little more time for yourself.

Find positives in your relationship
Looking after someone can change your relationship with them. Sometimes you may feel close and connected but at other times you may feel angry and irritated. It can help to talk openly and honestly to find way of coping together. Try to:
• Think of yourself as their friend, partner or family member first and foremost
• Talk together about how to strengthen positive parts of your relationship
• Do nice things together as well as day to day responsibilities.
Take a break and make time for yourself
Try and take a break, especially if you are worried about your own mental health. You may not be able to take a break every time you need one but it's important to have some time that's yours. The Carer's Trust has more information about the help you can get to take a break.
You may need an hour or two to clear your head or a day to help you feel more rested. You could go out, take a bath or turn your phone off for an agreed period of time. Try to make time for things you enjoy. If possible, try and plan regular breaks into your routine. This can help you make plans in advance, give you something to look forward to and make sure the person you look after knows what to expect.
Get enough sleep
Lack of sleep can make it more difficult to cope with day to day challenges and can make stress and depression worse. Have a look at our pages on how to cope with sleep problems.
Look after your physical health
It's important to try and make time to look after your physical health as best you can. Try and eat as healthily as you can and do some kind of regular physical activity. Our information pages on food and mood and physical activity has suggestions to help you fit things into a busy daily routine.
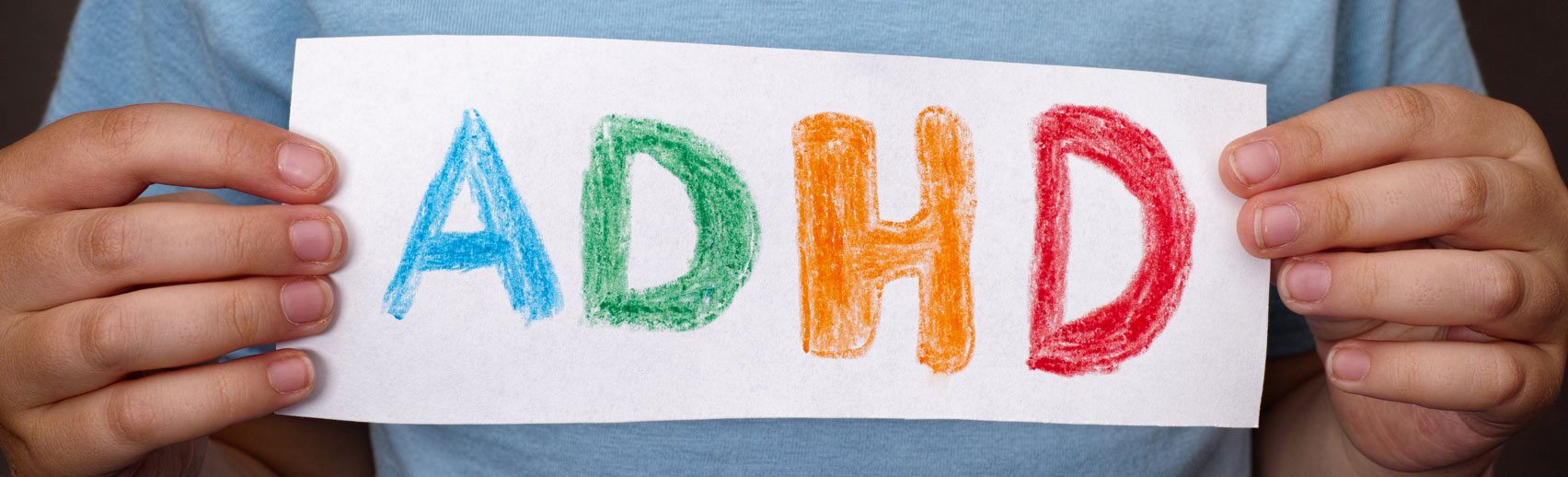
Imagine waking up in the morning and not being able to remember what you did the day before or how to complete your daily tasks at work? This can be a confusing and a highly emotional experience.
More than 520,000 people in the UK have dementia caused by Alzheimer’s disease and this figure is set to rise.
The word ‘dementia’ describes a set of symptoms that may include memory loss and difficulties with thinking, problem-solving or language. These changes are often small to start with, but for someone with dementia they become severe enough to affect daily life.
This was the case for Stuart, who first came in contact with the Electrical Industries Charity (EIC) in 2018. Stuart worked as an IT modelling engineer for a Nuclear Generation Company and it was his HR advisor who got in touch with the EIC in September 2018 following concern regarding Stuart’s wellbeing, with particular relation to his cognitive function.
The EIC got in touch with Stuart to see how he was feeling and establish if he had a perspective of his situation and changes in his everyday life. The charity assessed what initial support stuart might need and he had a brain scan in November, however the results were unfortunately inconclusive as to the prognosis.

The Electrical Industries Charity understands how important a support network can be to someone who is struggling to deal with a diagnosis that has life changing implications, and for this reason the Charity launched the Employee Assistance Programme (EAP). The Charity’s Programme ensures that employees and their immediate family members have a shoulder to lean on at the most difficult times, by offering them vital support services including counselling, legal advice and financial assistance and grants.
Alzheimer’s disease is the most common cause of dementia and is the cause of 60–70% of all cases diagnosed. Alzheimer’s is a progressive disease and is described as a chronic neurodegenerative disease that usually starts slowly and gradually worsens over time. Alzheimer’s is a complex condition which not only affects the individual, but the family system.
Stuarts condition was progressively deteriorating, he was becoming more confused and was struggling to retain his short-term memory. It was difficult for Stuart to understand his health circumstance, and he felt increasingly frustrated by his inability to complete what were previously routine daily tasks i.e. accessing his work computer and remembering his pin number.
When a family member is diagnosed with Alzheimer's disease or other dementia, the effect on your entire family can be overwhelming. The diagnosis can trigger a range of emotions — including anger, fear, frustration and sadness. There also are many decisions to make about treatment, care, living arrangements, finances and end-of-life care.
One important objective the EIC focused on with Stuart and his family was in supporting Stuart during the diagnostic phase to ensure he still maintained decision making capacity. It is often the case that individuals diagnosed with cognitive degenerative diseases have their autonomous decision making removed, as they are deemed as lacking capacity, however, the concept of mental capacity is fluid. It should not be assumed that just because someone has dementia, they are unable (lack capacity) to make their own decisions. People with dementia should be supported in making their own decisions about their care and day to day life for as long as possible.
Stuart required regular assessments to establish what decision’s he had the capacity to make and those he didn’t. The EIC used a specialised questionnaire to ask Stuart direct questions relating to his care. This was an important step as it was essential to Stuarts involvement in determining his own care plan.
The charity initiated the intervention of the social services and got the Alzheimer’s support group involved. The EIC also sought advice regarding financial circumstances on behalf of the family and maintained open communication between Stuart’s employer and his family, specifically his brother.
The EIC were integral in helping to provide Stuart and his family with emotional support and arranged for Stuart to attend weekly therapy sessions. The charity recently provided funding for Stuart to visit a brain clinic for further assessment and a diagnosis of Alzheimer’s was finally made. Stuart is now living with his ex-partner and he is doing okay.
Thanks to support from the industry, every year the Electrical Industries Charity is able to offer hundreds of our industry colleagues both practical and emotional support during their time of need.
If you or someone you know is struggling to deal with a life-changing diagnosis and requires support, please contact the EIC support team: This email address is being protected from spambots. You need JavaScript enabled to view it. or 0800 652 1618.

Caring for someone can take its toll on your physical and mental health, social life, career and relationships. Taking time out to look after yourself is important if you’re to continue supporting yourself and the person you’re caring for. Here are some of the different types of support available.
• What is a carer’s assessment?
• What happens after you’ve been assessed?
• If you’re eligible for financial support
• If you’re not eligible for financial support
• Other support options available for carers
• Other information resources To access many of these services you’ll first need to complete a carer’s assessment.
To access many of these services you’ll first need to complete a carer’s assessment.
What is a carer’s assessment?
Whether you care for someone full time or just a few hours a week, share your caring role with others or do it all alone, you’re entitled to a carer’s assessment from your local authority.
It’s your chance to discuss with a social worker what help you might need with caring for a friend or relative:



This could be your partner, parent or other family member and perhaps you have been struggling on because that’s what you do. There are many organisations that can help and support you.
How can we help you?
Carers Trust is a major charity for, with and about carers. We work to improve support, services and recognition for anyone living with the challenges of caring, unpaid, for a family member or friend who is ill, frail, disabled or has mental health or addiction problems. Our vision is that unpaid carers count and can access the help they need to live their lives.
Anyone could be a carer – a 15-year-old girl looking after a parent with an alcohol problem, a 40-year-old man caring for his partner who has terminal cancer, or an 80-year-old woman looking after her husband who has Alzheimer's disease.

- Carers Trust's local Network Partners are carer services across the UK, offering information, advice, practical support and/or care in the home. Many of them, but not all, have services for young carers and young adult carers. Find your nearest one by searching on their website.
- The Children’s Society can also help you find a young carers service near you.
Find support to keep you, and the person you care for, healthy.
- It is important that you take care of your own health and wellbeing, even if you are busy looking after someone else's health.
- Find out more about emergencies, equipment, adaptions and telecare, and the support you can get from your pharmacy.
- If you find that caring is putting a strain on your relationships with your partner, friends and family, we have details of organisations that can help.
- Find out about support you can get when caring ends.
- Getting a break from caring may also help you stay well.
- Contact your local carer service to see how they can help you stay healthy.
- Also see Live Well on NHS Choices for help with your diet, stopping smoking, getting enough exercise, and coping with stress.

Six items that belong on a not-to-do list for those unsung heroes: caregivers.
"… the most striking research finding is a tendency for the partner’s quality of life to be worse than that of the patient."
The people who are least likely to be surprised by this finding are not just caregivers, but those who are in their care. The study focused on partners and spouses, but I'm certain that the finding would be the same when the relationship of caregiver and “cared-for” is parent/child, child/parent, sibling/sibling … or a host of other relationships. From my own personal experience, as well as from feedback from others, I’ve learned a lot about the life of a caregiver. If you’re a caregiver, here is my not-to-do list for you.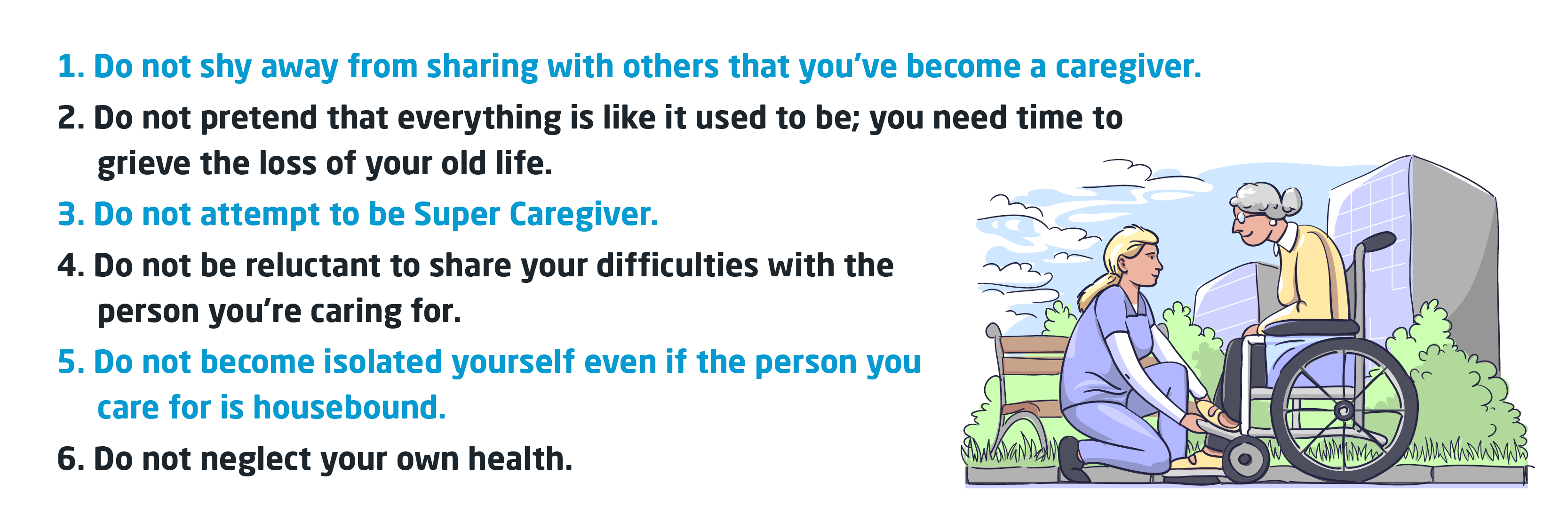
 Read More 7
Read More 7Can romantic relationships survive a chronic illness? If you or your loved one has recently been diagnosed, knowing how to handle possible changes can help you stay in love despite the emotional news of serious health problems or disease.
While facing and dealing with chronic illness is understandably frightening, that fear does not need to rule or ruin your life or your relationships. The most important first step you can take is agreeing to set a ground rule of total honest, open communication. To understand how this diagnosis will affect your relationship, you must first understand how this will alter your loved one.
Here are 5 ways living with a chronic disease or illness changes relationships and marriages, and what each of you can to do be prepared — and stay madly in love.
1. You Will Struggle to Keep the Illness from Defining You Both
2. Your Roles in the Relationship Will Change
3. Your Social Group Will Rearrange Itself, Usually for the Better
4. You Will Quarrel Differently
5. Your Focus and Priorities as a Couple Will Change

Living with dementia can have a big emotional, social, psychological and practical impact on a person. Many people with dementia describe these impacts as a series of losses and adjusting to them is challenging.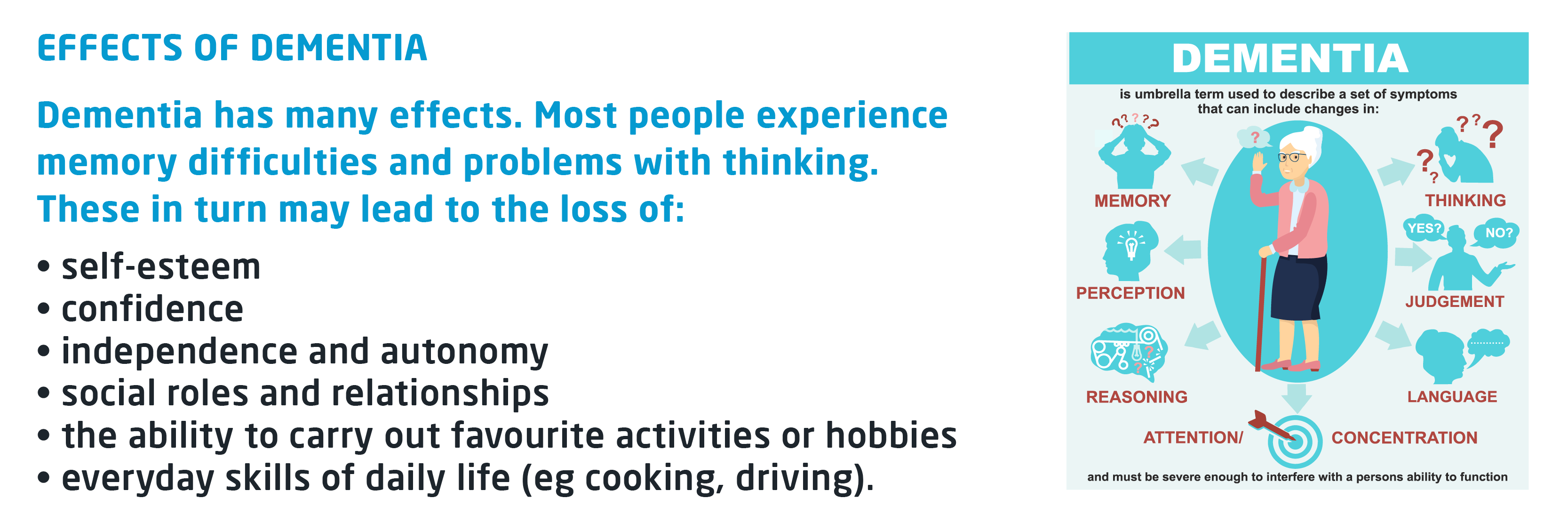
Despite all these things being lost, the person will still retain some of their abilities, and will still feel an emotional connection to people and their environment, even later on in the condition. Dementia will affect a person's day-to-day life and they may need to adapt how they do things. When supporting the person, there are approaches carers can take that can reduce the impact of these practical difficulties and help the person maintain a sense of normality for as long as possible. This will help the person to feel independent and maintain their self-esteem.
Communicating
People with dementia often experience difficulties communicating - for example, problems with finding the right word or following a conversation. Difficulties with communication may cause a person with dementia to lose confidence or withdraw from social situations. Families, friends and carers may find that these difficulties are frustrating and can increase stress.
Losing independence
A person with dementia may gradually lose their independence and become more reliant on the care and support of others around them. This can be a hard change to make and can be distressing for everyone involved. It is important that, where possible, families, friends and carers support the person to do things for themselves rather than 'taking over'. This increases the person's wellbeing and helps maintain their dignity, confidence and self-esteem, rather than making them feel helpless or worthless.
Decision-making
A person's ability to make decisions for themselves is called 'mental capacity' (often just 'capacity'). It means being able to weigh up different options, decide on one and communicate the decision. A person with dementia may eventually lose capacity to make certain decisions (eg choices about finances), but it should always be assumed that a person has capacity unless it can be shown otherwise.
Read More Here:
• The practical impact of dementia
• The psychological and emotional impact of dementia
• Coping with dementia
• Carers: looking after yourself when supporting someone with dementia
• Understanding and supporting a person with dementia - other resources
There are many positive things about caring. These include learning new skills, building on existing ones, strengthening relationships, having a sense of pride in what you are doing, and supporting someone who is important to you. And just because a person has dementia, it doesn’t mean there won’t still be good times for you to share. However, caring can also be both physically and mentally exhausting. It affects every part of your life and can make you feel isolated, stressed and sometimes even depressed.
You may also have your own physical and mental health needs, which you and others might overlook when you are caring for someone else. Everyone will experience caring in their own way. There may be days when you feel like you can cope well, and others when you cannot. You may find that there are some aspects of caring you can manage easily, while others prove more difficult. This can change from day to day.
Managing different priorities
You may often be faced with many different things you need to do at once. This can be difficult to manage and can leave you feeling exhausted – both physically and mentally. Many carers feel torn between different responsibilities. You may be trying to care for children, look after someone who is unwell, or go to work, as well as caring for the person with dementia. As much as you may want to be able to manage everything, it is not always possible. It is important to remember that you are only one person and you cannot do everything. Try to focus on what is most important and don’t be too hard on yourself about the things you can’t manage.

As the person’s condition progresses, their needs and abilities will change. You’ll need to learn to cope with this and adapt to these changes. It can often feel like you’re having to start all over again. It can be very difficult to see the person you care for struggling with things they used to be able to do. It is important to focus on what the person can still do and support them to do these things. Try not to focus on what they can’t do.
Dealing with difficult emotions
One of the most difficult things about caring for a person with dementia is the range of emotions you experience. You may feel frustrated or burnt out. You may be angry and wonder ‘Why me?’ You may feel isolated and cut off from the world. Or you may feel guilty for thinking about yourself instead of the person you care for. There may be times when you feel that you no longer love, or even like, the person you are caring for. Maybe you worry that you are only caring for the person out of a sense of duty. These are all very common reactions to caring for a person with dementia. Many other carers will be feeling the same as you do, and you shouldn’t be ashamed about how you feel. But if you don’t learn to deal with them, these feelings can have a negative impact on many parts of your life. They can affect your wellbeing and the wellbeing of the person you’re caring for, so it is important to address them.
Read More Here:
• Carers: looking after yourself
• Getting help and support as a carer
• Caring in the later stages
• Other resources for carers
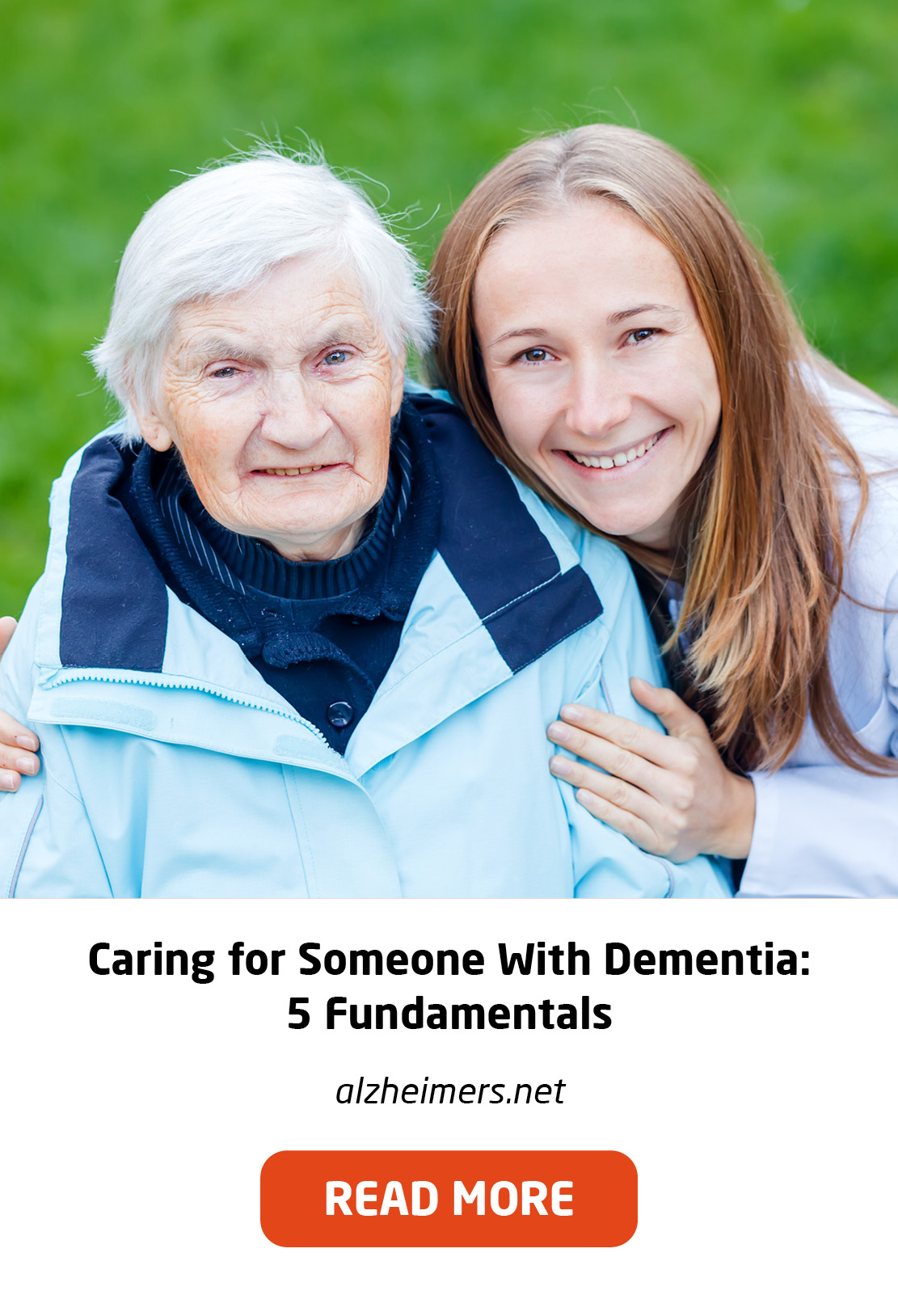
Caring for a loved one with dementia poses many challenges for families and caregivers. People with dementia from conditions such as Alzheimer’s and related diseases have a progressive biological brain disorder that makes it more and more difficult for them to remember things, think clearly, communicate with others, and take care of themselves. In addition, dementia can cause mood swings and even change a person’s personality and behaviour.
We aren’t born knowing how to communicate with a person with dementia—but we can learn. Improving your communication skills will help make caregiving less stressful and will likely improve the quality of your relationship with your loved one. Good communication skills will also enhance your ability to handle the difficult behaviour you may encounter as you care for a person with a dementing illness.
Ten Tips for Communicating with a Person with Dementia

Attention deficit hyperactivity disorder (ADHD) is a behavioural disorder that includes symptoms such as inattentiveness, hyperactivity and impulsiveness.
Symptoms of ADHD tend to be noticed at an early age and may become more noticeable when a child's circumstances change, such as when they start school. Most cases are diagnosed when children are 6 to 12 years old. The symptoms of ADHD usually improve with age, but many adults who were diagnosed with the condition at a young age continue to experience problems. People with ADHD may also have additional problems, such as sleep and anxiety disorders.
Living with attention deficit hyperactivity disorder (ADHD)
Looking after a child with ADHD can be challenging, but it's important to remember that they cannot help their behaviour.
Some issues that may arise in day-to-day life include:
• getting your child to sleep at night
• getting ready for school on time
• listening to and carrying out instructions
• being organised
• social occasions
• shopping
Adults with ADHD may also find they have similar problems, and some may have issues with relationships or social interaction.
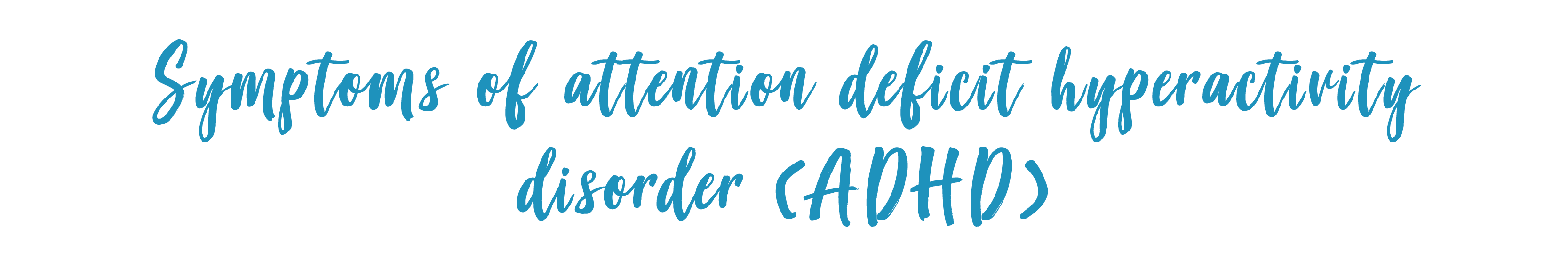
The symptoms of attention deficit hyperactivity disorder (ADHD) can be categorised into 2 types of behavioural problems: inattentiveness, and hyperactivity and impulsiveness.
Symptoms in children and teenagers
The symptoms of ADHD in children and teenagers are well defined, and they're usually noticeable before the age of 6. They occur in more than 1 situation, such as at home and at school. These symptoms can cause significant problems in a child's life, such as underachievement at school, poor social interaction with other children and adults, and problems with discipline.
These symptoms can cause significant problems in a child's life, such as underachievement at school, poor social interaction with other children and adults, and problems with discipline.
Related conditions in children and teenagers with ADHD
Although not always the case, some children may also have signs of other problems or conditions alongside ADHD, such as:
- Anxiety Disorder – which causes your child to worry and be nervous much of the time; it may also cause physical symptoms, such as a rapid heartbeat, sweating and dizziness
- Oppositional Defiant Disorder (ODD) – this is defined by negative and disruptive behaviour, particularly towards authority figures, such as parents and teachers
- Conduct Disorder – this often involves a tendency towards highly antisocial behaviour, such as stealing, fighting, vandalism and harming people or animals
- Depression
- Sleep Problems – finding it difficult to get to sleep at night, and having irregular sleeping patterns
- Autistic Spectrum Disorder (ASD) – this affects social interaction, communication, interests and behaviour
- Epilepsy – a condition that affects the brain and causes repeated fits or seizures
- Tourette's Syndrome – a condition of the nervous system, characterised by a combination of involuntary noises and movements (tics)
- Learning Difficulties – such as dyslexia

Difference between ADHD and ADD (Attention Deficit Disorder)
- The symptoms of attention deficit hyperactivity disorder (ADHD) can be categorised into 2 types of behavioural problems: inattentiveness, and hyperactivity and impulsiveness.
- Most people with ADHD have problems that fall into both these categories, but this is not always the case.
- For example, some people with the condition may have problems with inattentiveness, but not with hyperactivity or impulsiveness.
- This form of ADHD is also known as attention deficit disorder (ADD). ADD can sometimes go unnoticed because the symptoms may be less obvious.
Symptoms in adults
By the age of 25, an estimated 15% of people diagnosed with ADHD as children still have a full range of symptoms, and 65% still have some symptoms that affect their daily lives. Some specialists say the way in which inattentiveness, hyperactivity and impulsiveness affect adults can be very different from the way they affect children. For example, hyperactivity tends to decrease in adults, while inattentiveness tends to get worse as the pressures of adult life increase.
Parents are often both saddened and angry all at the same time, feel a great deal of self-doubt in their parenting, and find themselves becoming frustrated saying things to their child they sincerely regret.
Many children and teenagers are diagnosed with ADHD. Parents are familiar with the list of symptoms and often get professionals to help their child modify their disorganisation, distractibility, and hyperactivity. But rarely are the parents given guidance on how to handle their own feelings about their child's problems and actions, and many parent-child arguments and conflicts ensue, which only worsen the child's shame and confusion.
Parents care deeply about their child but don't know what attitude or mindset to have when they are faced with their child's irritability, loss of emotional regulation and control, disorganized homework and clothing, loss and misplacement of articles and assignments, and erratic judgment.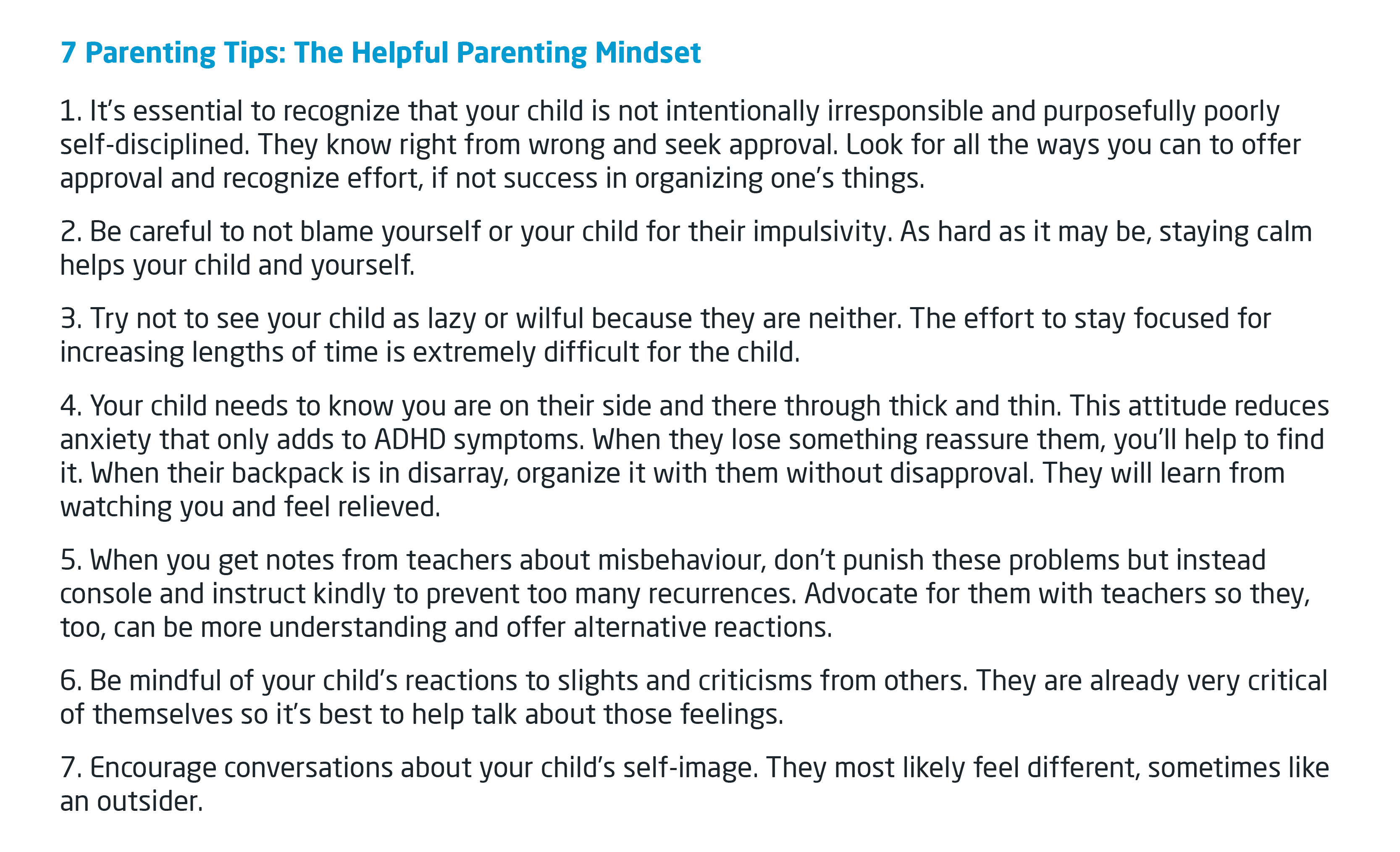 When you follow these tips, your attitude changes because you feel with your child in their battle with themselves. It improves their self-esteem as well as yours as a parent. This parental mindset helps them absorb new skills and temper emotions. That makes all the difference.
When you follow these tips, your attitude changes because you feel with your child in their battle with themselves. It improves their self-esteem as well as yours as a parent. This parental mindset helps them absorb new skills and temper emotions. That makes all the difference.

Raising a child with ADHD isn’t like traditional childrearing. Normal rulemaking and household routines can become almost impossible, depending on the type and severity of your child’s symptoms, so you’ll need to adopt different approaches. It can become frustrating to cope with some of the behaviours which result from your child’s ADHD, but there are ways to make life easier.
Parents must accept the fact that children with ADHD have functionally different brains from those of other children. While children with ADHD can still learn what is acceptable and what isn’t, their disorder does make them more prone to impulsive behaviour.
There are two basic principles of behaviour management therapy. The first is encouraging and rewarding good behaviour (positive reinforcement). The second is removing rewards by following bad behaviour with appropriate consequences, leading to the extinguishing of bad behaviour (punishment, in behaviourist terms). You teach your child to understand that actions have consequences by establishing rules and clear outcomes for following or disobeying these rules. These principles must be followed in every area of a child’s life. That means at home, in the classroom, and in the social arena.

Decide ahead of time which behaviours are acceptable and which are not
The goal of behavioural modification is to help your child consider the consequences of an action and control the impulse to act on it. This requires empathy, patience, affection, energy, and strength on the part of the parent. Parents must first decide which behaviours they will and won’t tolerate. It’s crucial to stick to these guidelines. Punishing a behaviour one day and allowing it the next is harmful to a child’s improvement. Some behaviours should always be unacceptable, like physical outbursts, refusal to get up in the morning, or unwillingness to turn off the television when told to do so.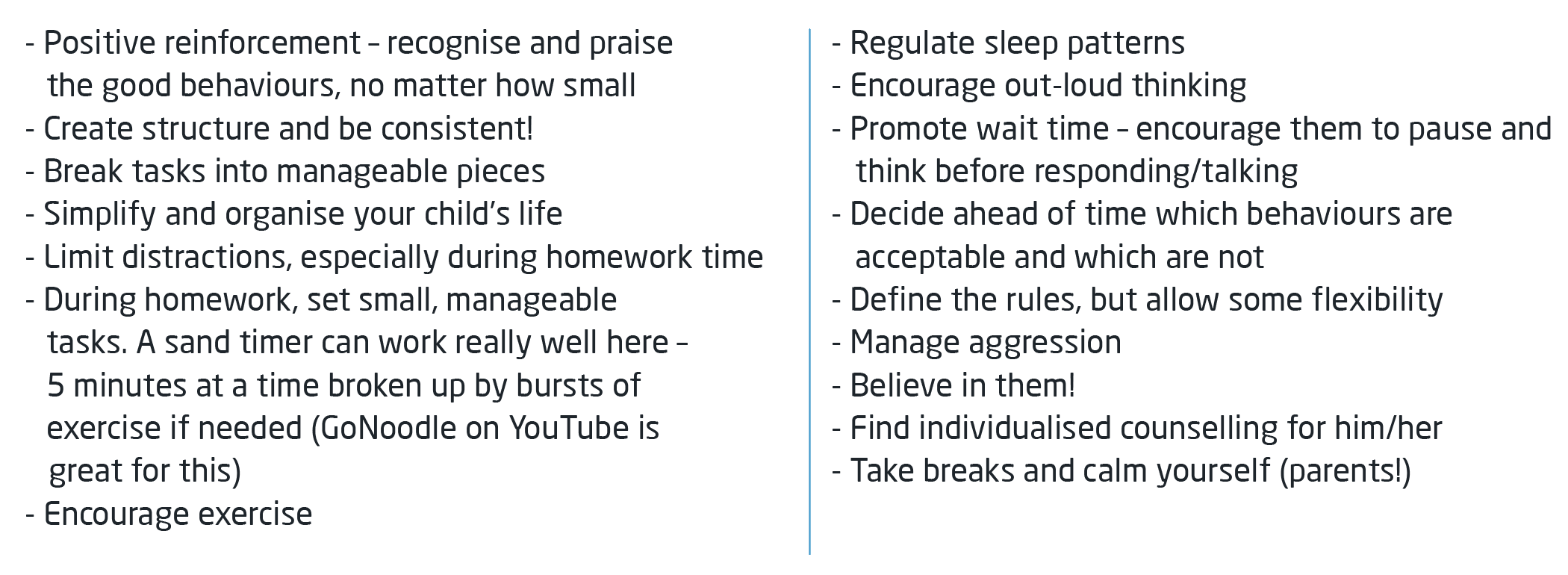

What is CAMHS?
CAMHS offers assessment and help to children, young people and their families with emotional, behavioural and mental health difficulties.
Do you think your child has a behavioural difficulty?

References:
1. https://www.mind.org.uk/information-support/helping-someone-else/carers-friends-family-coping-support/am-i-a-carer/
2. https://www.mind.org.uk/information-support/helping-someone-else/carers-friends-family-coping-support/looking-after-yourself/
3. https://www.moneyadviceservice.org.uk/en/articles/support-services-available-to-carers#help-is-at-hand
4. https://www.carersuk.org/news-and-campaigns/press-releases/facts-and-figures
5. https://carers.org/
6. https://www.psychologytoday.com/gb/blog/turning-straw-gold/201401/not-do-list-caregivers-the-chronically-ill
7. https://psychcentral.com/blog/5-ways-a-chronic-illness-can-affect-your-relationship
8. https://www.alzheimers.org.uk/get-support/help-dementia-care/understanding-supporting-person-dementia#content-start
9. https://www.alzheimers.org.uk/get-support/help-dementia-care/caring-for-person-dementia
10. https://www.caregiver.org/caregivers-guide-understanding-dementia-behaviors
11. https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/
12. https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/symptoms/
13. https://www.healthline.com/health/adhd/parenting-tips
14. https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/symptoms/
15. https://camhs.elft.nhs.uk/Who-we-help/ParentsCarers