The charity is adapting its support service to help industry members through this pandemic. We are providing regular updates for the industry and offering lots of useful information, advice and support links on issues that may be affecting you or your family members during COVID-19 such as:
Practical Support - Reducing personal debt, helpful advice for those who are worried about their and the person that they care for safety - Salary and more.
Employed and Self-employed support - Help and Guidance for employers who are looking to furlough employees or struggling with Covid-19 generally and more.
Mental Health support - Feeling the pressure to be productive? A useful toolkit to support your mental health during the pandemic, how to protect your mental health during the pandemic and more.
Housing support - The welfare team are supporting renters who need to write to their landlords in support for rent holidays and more.
Welfare benefit Support - If you are self-employed or lost your job because of COVID-19 consider applying for universal credit? And more.
Legal support – Advice for employees requiring legal support during the pandemic and more.
Self-Isolation - Guide for social distancing and more.
For all this information and more please visit our COVID-19 regular updates website page at the link below:


It is so important to keep track of our health and understand the intricacies of both our physical and mental health. This month we put the spotlight on women’s health and some of the things which affect women’s health in particular. We look at cervical and breast cancer, the leading cancers for women, as well as women’s mental health.

Maria works three days a week as a production line operative for an electrical manufacturer and distributor. She started to go through the menopause and was experiencing hot flushes, headaches, leg stiffness, night sweats which were affecting her sleep, as well as feeling very low and unmotivated. Her role involves a lot of physical work, including standing up for long periods of time, and her menopausal symptoms made working for long periods very uncomfortable.
For the first few months, Maria soldiered on and called in sick when she found it too difficult to go into work, but she felt guilty for doing so. She called the EIC who encouraged her open up to her manager, Tim, who was very understanding. He recommended she spoke with her GP to seek advice and was prescribed medication to help her through her menopause and reduce the discomfort she was experiencing. The EIC worked with Tim to support him in supporting Maria. He invited her to work flexible shifts, meaning she could split her shifts in half, or work one week on and one week off, to enable her to rest when needed. He also agreed to paid leave whenever she needed to attend a medical appointment and arranged fortnightly check-ins to make sure Maria was coping okay.
Tim created an area for Maria with a lower workbench to enable her to work whilst sitting down where possible. He also supplied a fan to help Maria when she was experiencing hot sweats. Maria felt valued by Tim as he respected her need for support and put everything, he could in place to enable her to feel comfortable in the workplace.
The Electrical Industries Charity can work alongside your employer to create a positive and supportive work environment for your changing needs – it all starts with reaching out. If you need assistance due to your altering lifestyle contact the support team on This email address is being protected from spambots. You need JavaScript enabled to view it.
or 0800 652 1618


Danielle is an electrical apprentice and started going to the gym 18 months ago. She had been over-weight as a teenager and was teased by others in her class. The gym started as an escape and she would go 3-4 times per week, but once she saw the results, she was achieving it quickly became a twice-a-day obsession.
Danielle would feel incredibly guilty or depressed if a workout was skipped and would find the time to exercise no matter the expense. She worked out despite being injured from a previous gym session which made the injury worse, causing great distress as she knew she couldn’t return until she was fit to do so. By the time her family had realised what was happening, Danielle had already developed an unhealthy relationship with her body and food. She was counting every calorie on a food-tracking app, never allowing herself a ‘cheat’ day. She would skip events with her friends and family to go to the gym and began purging after meals and using laxatives to lose weight even faster.
When Danielle’s family put her in touch with the EIC for support, she was still in the mindset that she needed to lose weight. Danielle was referred for Dialectical Behaviour Therapy (DBT), a branch of Cognitive Behavioural Therapy which is proven to be successful in supporting those with an eating disorder. After 12 months of charity sourced and funded DBT, Danielle has developed a much healthier relationship with food and exercise and is feeling much happier in herself.
The Electrical Industries Charity are here to support you whatever stage in your career you are at. The charity are dedicated to supporting apprentices and are passionate about championing positive mental and physical health. If you are struggling with an eating disorder or know someone who may be then please contact the welfare team on This email address is being protected from spambots. You need JavaScript enabled to view it. or 0800 652 1618.

Breast cancer is the most common type of cancer in the UK. Most women diagnosed with breast cancer are over the age of 50, but younger women can also get breast cancer. About 1 in 8 women are diagnosed with breast cancer during their lifetime. There's a good chance of recovery if it's detected at an early stage.
What is breast cancer and how does it start?
Breast cancer occurs when abnormal cells in the breast grow in an uncontrolled manner. It occurs in both men and woman, but women are at greater risk due to their breast development and lifelong exposure to oestrogens. Cells that grow abnormally can form tumours. Breast cancer occurs when breast tumours spread. There is generally a long period between breast tissue changes and development of breast cancer.


Breast cancer is a diverse group of diseases. Sub-types have different properties in relation to hormone sensitivity and invasiveness as well as menopausal status. Invasive ductal breast cancer occurs in epithelial cells that line the breast ducts and accounts for around 80% of all breast cancers. Invasive lobular breast cancer occurs in lobes and accounts for around 10% of breast cancers. Hormone receptor positive cancers are those that grow in response to high concentrations of oestrogen, progesterone and/or human epithelial growth factor 2 (HER2). The most common of these is oestrogen receptor positive cancer. Cells from these tumours produce additional oestrogen receptors and depend on oestrogen to grow. Triple negative breast cancer is a rarer type of breast cancer which does not have additional receptors for oestrogen, progesterone or HER2. It is more common in younger women and tends to be more aggressive.
In situ breast carcinoma (also called non-invasive breast cancer) is an early form of breast cancer, which remains localised to the breast. The most common form is ductal carcinoma in situ (DCIS); if left untreated DCIS may become invasive. Another common non-invasive breast cancer is lobular carcinoma in situ (LCIS). This type of carcinoma is not cancerous (so does not spread), although its presence is correlated with an increased chance of developing cancer at a later stage.
Breast cancer is the most common cancer in the UK with one woman diagnosed every 10 minutes.
Around 55,000 women and 370 men are diagnosed with breast cancer every year in the UK
- In England, every year around 46,000 people are diagnosed with breast cancer.
- In Scotland, every year around 4,700 people are diagnosed with breast cancer.
- In Wales, every year around 2,900 people are diagnosed with breast cancer.
- In Northern Ireland, every year around 1,400 people are diagnosed with breast cancer.
- A further 7,000 people are diagnosed with DCIS (ductal carcinoma in situ), an early form of breast cancer, in the UK every year.
Breast cancer facts and figures
- One in seven women in the UK will develop breast cancer in their lifetime.
- Eight out of 10 cases of breast cancer are diagnosed in women aged 50 and over.
- One-quarter of cases are diagnosed in women aged 75 and over.
- Just over 10,000 women are diagnosed with breast cancer under the age of 50 every year in the UK.
Of these, nearly 8,000 women will be in their 40s. - Around 2,200 women in the UK are diagnosed aged 39 or under, or just 4% of all cases.
- Almost nine in 10 (87%) women survive breast cancer for five years or more.
- Breast cancer survival is improving and has doubled in the past 40 years in the UK.
- The proportion of breast cancer cases that can be prevented is estimated to be between 23%-37%.


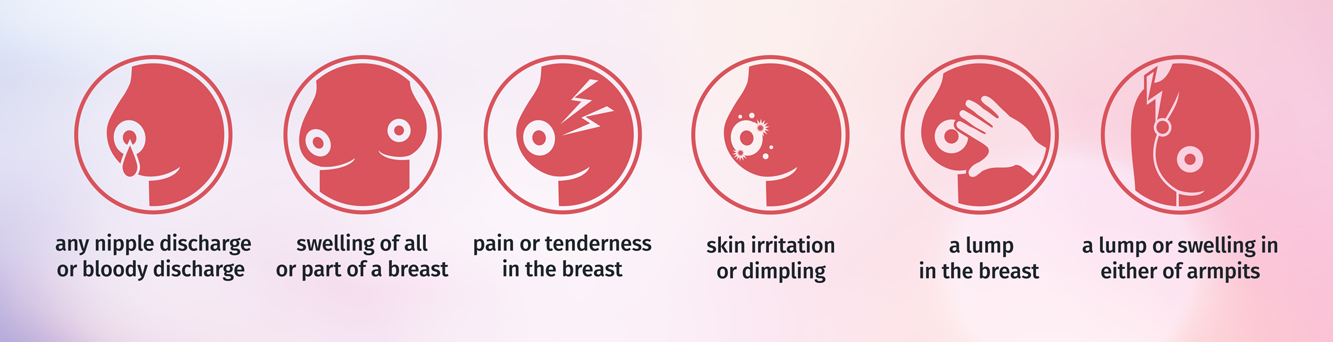
Breast cancer can have several symptoms, but the first noticeable symptom is usually a lump or area of thickened breast tissue. Most breast lumps are not cancerous, but it's always best to have them checked by a doctor. You should also see a GP if you notice any of these symptoms:
- A change in the size or shape of one or both breasts
- Discharge from either of your nipples, which may be streaked with blood
- A lump or swelling in either of your armpits
- Dimpling on the skin of your breasts
- A rash on or around your nipple
- A change in the appearance of your nipple, such as becoming sunken into your breast
- Breast pain is not usually a symptom of breast cancer.
It’s important to check your breasts for lumps, bumps or anything out of the ordinary.
Check regularly
We believe boob checking should be a monthly habit, so that you will notice any unusual changes quickly. By checking on a regular basis, you will also build confidence of knowing what is normal for you each month. Everyone has to start somewhere, so don’t worry if you’re not feeling confident straight away.
Know what’s normal for you
Being breast aware simply means knowing what is normal for your boobs or pecs. If you have periods, it’s likely you’ll find that your boobs will naturally change as part of your cycle each month. It is important to get to know the normal rhythm of your boobs so you will be able to detect anything unusual quickly.
Look and Feel
Many of the signs and symptoms of breast cancer are changes you would only notice by looking at the appearance of your boobs. We recommend coppin’ a feel and taking a look during your checks
Remember your Collarbone and armpits
Breast tissue isn’t only found in your boobs. It reaches all the way up to your collarbone and underneath your armpit so this whole area should be checked each time too. This is the same for both men and women.
If in doubt, get it checked out
Your doctor is the only person who can refer you for further examination so we encourage people to visit their doctor after a week of monitoring the symptom if it doesn’t go away.
Here are some things to look out for when checking your breasts
As a woman over 50 within the UK you will begin to receive letters regarding breast cancer screenings
What happens during breast screening?
Breast screening involves having an X-ray (mammogram) at a special clinic or mobile breast screening unit. This is done by a female health practitioner. Your breasts will be X-rayed 1 at a time. The breast is placed on the X-ray machine and gently but firmly compressed with a clear plate. Two X-rays are taken of each breast at different angles. If you have a cancerous growth in your breasts you will be tested further and a doctor will find out more about the growth and position of the cancer.
This is called staging
A doctor decides the grade of the cancer by how the cancer cells look under the microscope. This gives an idea of how quickly the cancer might grow or spread. Knowing the stage and grade helps your doctors plan the best treatment for you. You will then receive treatment dependent on the stage of cancer. This treatment can range from mastectomy to chemotherapy, radiotherapy or hormonal therapy.


If you are diagnosed with breast cancer there is support out there for you. We work alongside Macmillan cancer support to help you during the most difficult of times.
Macmillan Cancer Support Line: The Macmillan Support Line offers confidential support to people living with cancer and their loved ones. If you need to talk, we'll listen. 0808 808 00 00 - 7 days a week, 8am - 8pm
Email / Chat online: 7 days a week, 8am - 8pm
Online Community: An anonymous network of people affected by cancer which is free to join. Share experiences, ask questions and talk to people who understand.
Help in your area: What's going on near you? Find out about support groups, where to get information and how to get involved with Macmillan where you live.
There is a multitude of charitable organisations which can help you

If a friend or family member has been diagnosed with breast cancer, there are a number of things you can do to help or support them.
- Practical support:
Many people want to carry on doing as much as possible during their treatment. However, side effects can often make it more difficult to continue with everyday tasks and asking for help is not always easy. Knowing how to help can sometimes be difficult. As well as thinking about what your friend or family member might need help with, it’s important to think about what you’re able to do and how much time you’re able to commit. Offering specific help means both parties understand what’s on offer. For example, rather than saying ‘What can I do for you?’ it might be better to say ‘Would you like me to pick the children up from school tomorrow?’.
Things you might offer to help with include:
- cleaning and vacuuming
- clothes washing and ironing
- gardening
- cooking meals for freezing
- transport to and from hospital appointments
- taking children to or from school
- babysitting
- Some people may be reluctant to accept help or even feel embarrassed about the help that’s being offered. This can sometimes feel hurtful, but it’s important to some people to maintain a sense of normality and to continue to do things even when doing so is very difficult. - Emotional support:
Most people are shocked to hear they have breast cancer and experience many different emotions including anger, fear, sadness and depression. Feelings can change from day to day and even hour to hour. It’s often difficult to know what to say and how best to support someone. Just being alongside someone and allowing them to express how they’re feeling is probably one of the most important ways of supporting them. Try not to be afraid of tears that may be shed – it may be a helpful way for your friend or relative to express how they’re feeling. If it’s appropriate, holding hands or giving them a hug is a useful way of showing your support.
If someone is feeling angry about their diagnosis they may direct this at you. This can be hurtful – particularly if you’re trying to support them. But try to remember this is often because they’re upset about having cancer, rather than being upset with you. Listening to your friend or relative talk about how they’re feeling can sometimes be difficult or distressing, but it might be really helpful to them to express how they’re feeling. - Support for you:
Supporting a friend or relative can be very demanding and upsetting. To be able to continue to support your friend or relative, you need to look after yourself. Depending on how involved you are it’s important to eat well, get some regular exercise and a good night’s sleep and have some time to yourself. If you’re finding it difficult to do these things and are feeling overwhelmed, let a friend, family member or your GP know.
There are a number of places you can turn to for additional support, including:
- Breast Cancer Now’s Helpline, online Forum and Someone Like Me service
- Samaritans
- Carers UK


It is important to remember that there are no set rules and every friendship is different. Be sure to think about your unique dynamic and let that guide you as you try to support your friend. Keep it simple. Remember that often the little things mean the most.
Take Time to Prepare Yourself
Here are some things to consider before talking to a friend who has cancer:
- Process your own feelings beforehand. Learning that a friend has cancer can be difficult news to hear. Take time to acknowledge and cope with your own emotions about the diagnosis before you see him or her. This way, you can keep the focus on your friend.
- Learn about the diagnosis. Your friend may not want to talk about the details for many reasons. It can be physically and emotionally tiring to repeat the same information to different people. If possible, the person’s spouse or a mutual friend may be able to give you the basics. Write it down and repeat it back to them to be sure you have the correct information. If there is information that is unknown or not shared, do not push for more.
- Think about it from your friend’s perspective. Remember a time when you were scared or felt sick. Think about what it felt like. What did you want to talk about? How did you want to be treated? You may also want to prepare yourself for changes in your friend’s appearance. Fatigue, weight loss, and hair loss are common side effects of cancer and many treatments. Start your visit by saying “It’s good to see you” instead of commenting on any physical changes.
Although each person with cancer is different, here are some general suggestions for showing support:
- Ask permission. Before visiting, giving advice, and asking questions, ask if it is welcome. Be sure to make it clear that saying no is perfectly okay.
- Make plans. Do not be afraid to make plans for the future. This gives your friend something to look forward to, especially because cancer treatment can be long and tiring.
- Be flexible. Make flexible plans that are easy to change in case your friend needs to cancel or reschedule.
- Laugh together. Be humorous and fun when appropriate and when needed. A light conversation or a funny story can make a friend’s day.
- Allow for sadness. Do not ignore uncomfortable topics or feelings.
- Check in. Make time for a check-in phone call. Let your friend know when you will be calling. Also, let your friend know that it is okay not to answer the phone.


Survival for breast cancer is generally good, particularly if you are diagnosed early. This is probably because of screening, early diagnosis and improved treatment. Survival depends on many different factors. So no one can tell you exactly how long you will live. It depends on your:
- Type and stage of cancer
- Level of fitness
- Previous treatment
Survival by stage:
No UK-wide statistics are available for different stages of breast cancer or individual treatments. These figures are for survival by stage for women in England, five years after diagnosis. These are from women diagnosed between 2013 and 2017 and followed up to 2018.
Stage 1 - Most women (around 98%) will survive their cancer for 5 years or more after diagnosis.
Stage 2 - Around 90 out of 100 women (around 90%) will survive their cancer for 5 years or more after diagnosis.
Stage 3 - More than 70 out of 100 women (more than 70%) will survive their cancer for 5 years or more after diagnosis.
Stage 4 - Around 25 out of 100 women (around 25%) will survive their cancer for 5 years or more after they are diagnosed. The cancer is not curable at this point, but may be controlled with treatment for some years. It is important to remember that for the most part a breast cancer diagnosis does not mean an end-of-life diagnosis.

Young cervical cancer diagnosis:
Cervical cancer develops in a woman's cervix. It mainly affects sexually active women aged between 30 and 45. Cervical cancer is when abnormal cells in the lining of the cervix grow in an uncontrolled way. The cervix is part of the female reproductive system. It is the opening to the vagina from the womb. Around 3,200 women are diagnosed with cervical cancer in the UK each year. That’s nearly 9 cases diagnosed every day.
Cervical cancers and cervical pre-cancers are classified by how they look in the lab s with a microscope. The main types of cervical cancers are squamous cell carcinoma and adenocarcinoma. Most (up to 9 out of 10) cervical cancers are squamous cell carcinomas. These cancers develop from cells in the exocervix. Squamous cell carcinomas most often begin in the transformation zone (where the exocervix joins the endocervix). Most of the other cervical cancers are adenocarcinomas. Adenocarcinomas are cancers that develop from glandular cells. Cervical adenocarcinoma develops from the mucus-producing gland cells of the endocervix. Less commonly, cervical cancers have features of both squamous cell carcinomas and adenocarcinomas. These are called adenosquamous carcinomas or mixed carcinomas.
Cervical cancer statistics:
- In females in the UK, cervical cancer is the 14th most common cancer, with around 3,100 new cases in 2017.
- Cervical cancer accounts for 2% of all new cancer cases in females in the UK (2017).
- Cervical cancer in England is more common in females living in the most deprived areas.
- Cervical cancer is more common in White females than in Asian females, but similar to Black females, but Asian and Black females are similar to each other.
- An estimated 34,800 women who had previously been diagnosed with cervical cancer were alive in the UK at the end of 2010.
- There are around 850 cervical cancer deaths in the UK every year, that's more than 2 every day (2015-2017).
- In females in the UK, cervical cancer is the 19th most common cause of cancer death, with around 850 deaths in 2017.
The symptoms of cervical cancer are not always obvious, and it may not cause any at all until it's reached an advanced stage.
This is why it's very important to you attend all your cervical screening appointments.
Unusual Bleeding:
In most cases, abnormal vaginal bleeding is the first noticeable symptom of cervical cancer.
This includes bleeding:
• during or after sex
• between your periods
• after you have been through the menopause
Visit your GP for advice if you experience any type of abnormal vaginal bleeding.
Other Symptoms:
Other symptoms of cervical cancer may include pain and discomfort during sex, unusual or unpleasant vaginal discharge, and pain in your lower back or pelvis.
Advanced cervical cancer:
If the cancer spreads out of your cervix and into surrounding tissue and organs, it can trigger a range of other symptoms, including:
• pain in your lower back or pelvis
• severe pain in your side or back caused by your kidneys
• constipation
• peeing or pooing more often than normal
• losing control of your bladder (urinary incontinence) or losing control of your bowels (bowel incontinence)
• blood in your pee
• swelling of one or both legs
• severe vaginal bleeding


Cervical screening (a smear test) checks the health of your cervix. The cervix is the opening to your womb from your vagina. It's not a test for cancer, it's a test to help prevent cancer. All women and people with a cervix aged 25 to 64 should be invited by letter. During the screening appointment, a small sample of cells will be taken from your cervix. The sample is checked for certain types of human papillomavirus (HPV) that can cause changes to the cells of your cervix. These are called "high risk" types of HPV. If these types of HPV are not found, you do not need any further tests.
If these types of HPV are found, the sample is then checked for any changes in the cells of your cervix. These can then be treated before they get a chance to turn into cervical cancer. You'll get your results by letter, usually in about 2 weeks. It will explain what happens next.
HPV and Cervical Cancer Prevention:
Currently, the national NHS HPV vaccination programme uses a vaccine called Gardasil. Gardasil protects against 4 types of HPV: 6, 11, 16 and 18. Between them, types 16 and 18 are the cause of most cervical cancers in the UK (more than 70%).
From September 2019, the first dose of the HPV vaccine will be routinely offered to girls and boys aged 12 and 13 in school Year 8. The second dose is normally offered 6 to 12 months after the first (in school Year 8 or Year 9). People who miss either of their HPV vaccine doses should speak to their school immunisation team or GP surgery and make an appointment to get up-to-date as soon as possible. It's important to have both doses of the vaccine to be fully protected. People who were eligible for HPV vaccination in school Year 8 but who missed it can still be vaccinated on the NHS up to their 25th birthday. People who start the HPV vaccination after the age of 15 will need 3 doses as they do not respond as well to 2 doses as younger people do.
Even if you have had the HPV vaccine, it is still incredibly important to still attend regular smear tests. You will usually have your smear test at your GP or sexual health clinic. If you have questions or worries, let the nurse or doctor know. They will try to make you comfortable.
When you are ready you:
- Undress from the waist down
- Lie down on your back on an examination couch
- Will be asked to lie with your knees bent and feet flat on the couch or with your feet together and knees apart. Some clinics have a couch with leg supports.
The nurse or doctor will:
- Gently put an instrument called a speculum into your vagina
- Use this instrument to open the vagina just enough to see your cervix
- Sweep a small soft plastic brush over the cervix to take the sample of cells.
- The test takes less than five minutes. It should not hurt but sometimes it can feel uncomfortable.
Try not to put your smear tests off, you may feel embarrassed or think they’re uncomfortable but they are your best chance of preventing cervical cancer.
If your cervical screening test shows abnormal cells, you may have a different test to look closely at your cervix. This is called a colposcopy. This test uses a microscope called a colposcope to look closely at your cervix. The colposcopy shows abnormal areas of the cervix and how abnormal the cells there are. Sometimes the doctor or nurse can see during the test that the cells are very abnormal but it is not clear how serious the changes are.
They may:
- Offer you treatment to remove these cells straight away
- Take a small sample (biopsy) off the cells to check if you need treatment.
- If you have a biopsy, results may take 2 or 3 weeks. Ask your doctor or nurse when you will get the results.
Before any treatment, you should be given time and information to make a decision. If you have questions, want more time or are not sure, the treatment can always be done another day. Your doctor or nurse will only offer treatment if they are sure the cells are very abnormal and there is a risk of cancer developing.


For cervical cancer support you can contact Macmillan cancer support or go to Jo’s Cervical Cancer Trust. You might have a number of different feelings when you're told you have cancer. You may feel shocked and upset.
You might also feel:
- Numb
- Frightened and uncertain
- Confused
- Angry and resentful
- Guilty
You may have some or all of these feelings. Or you might feel totally different. Everyone reacts in their own way. Sometimes it's hard to take in the fact that you have cancer at all. Experiencing different feelings is a natural part of coming to terms with cancer. All sorts of feelings are likely to come and go. Talking to your friends and relatives about your cancer can help and support you. But some people are scared of the emotions this could bring up and won’t want to talk. They might worry that you won't be able to cope with your situation. It can strain relationships if your family or friends don't want to talk. But talking can help increase trust and support between you and them.
Help your family and friends by letting them know if you would like to talk about what’s happening and how you feel. You might find it easier to talk to someone outside your own friends and family. Macmillan have cancer information nurses you can call on their freephone
0808 800 4040, from 9am to 5pm, Monday to Friday.
Or you may prefer to see a counsellor. Specialist nurses can help you if you’re finding it difficult to cope or if you have any problems. They can get you the help you need. They can also give you information. Cervical cancer and its treatment can cause physical problems that may affect how you feel about yourself. Your treatment may mean that you can no longer become pregnant. This can be very difficult to cope with if you were hoping to have children in the future. Even if you had already been through the menopause, having surgery to remove your womb can still be very upsetting. Your doctor will talk to you about how treatment may affect your fertility and what the options are. It might be possible to store your eggs or embryos before treatment starts.
Practical things you and your family might need to cope with include:
- Money matters
- Financial support, such as benefits, sick pay and grants
- Work issues
- Childcare
Talk to your doctor or specialist nurse to find out who can help. Getting help early with these things can mean that they don’t become a big issue later. As with most cancers, survival for cervical cancer is improving. One-year age-standardised net survival has increased from 74% during 1971-1972 to 83% during 2010-2011 in England and Wales


Ovarian Cancer can be one of the trickier cancers to spot and diagnose in women and because of the this it is the 5th highest cause of cancer death in women. 8 out of 10 have symptoms early and 4 out of 5 will be misdiagnosed. 1 in 4 wait 6 months for a correct diagnosis.
These are quite shocking figures, so what are the symptoms?
Common symptoms include:
- Increase in tummy size
- Bloating
- Abdominal/back/pelvic pain
- Needing to pee more often or urgently
- Bowel changes
- Fatigue
Symptoms can be vague and variable.
But any of the following symptoms could also be an indication, if they last longer than 2 weeks, steadily worsen, are frequent or unusual:
- Feeling full after eating only a few bites or loss of appetite
- Diarrhoea, constipation, bowel or rectum feels full, change in bowel habits, constant urge to have a bowel movement, painful or burning bowel movements, rectal pain, painful defecation
- Bloating, distension of abdomen, clothes around the waist feel too tight, feel an abdominal mass
- Weight loss not because of dieting
- Nausea, vomiting, heartburn, gas, burping, indigestion
- Increased urinary frequency, need to urinate urgently, pressure on the bladder, leaking urine, burning sensation when urinating, need to urinate but unable to do so, unable to empty bladder completely, feeling full after urinating
- Vaginal discharge, bleeding, spotting, deep pain on intercourse
- Discomfort or pain in abdomen, pelvic region, or lower back

The menopause is when a woman stops having periods and is no longer able to get pregnant naturally. Periods usually start to become less frequent over a few months or years before they stop altogether. Sometimes they can stop suddenly. The menopause is a natural part of ageing that usually occurs between 45 and 55 years of age, as a woman's oestrogen levels decline. In the UK, the average age for a woman to reach the menopause is 51. But around 1 in 100 women experience the menopause before 40 years of age. This is known as premature menopause or premature ovarian insufficiency. Most women will experience menopausal symptoms. Some of these can be quite severe and have a significant impact on your everyday activities.
Common symptoms include:
- Hot flushes
- Night sweats
- Vaginal dryness and discomfort during sex
- Difficulty sleeping
- Low mood or anxiety
- Reduced sex drive (libido)
- Problems with memory and concentration
Menopausal symptoms can begin months or even years before your periods stop and last around 4 years after your last period, although some women experience them for much longer.

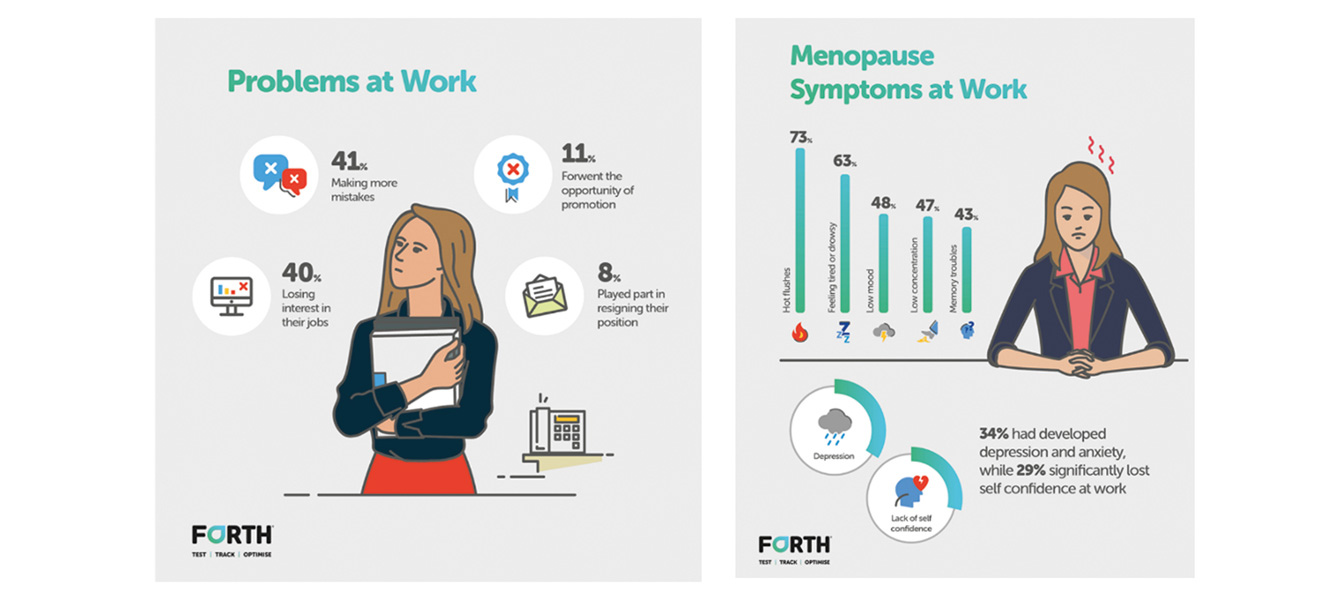
A survey of 1000 women, all aged 45 or over, based across the UK determined how significantly, and in what ways, women in both full time and part time employment are affected by symptoms of the menopause, and what policies and procedures are currently in place within organisations to provide help and support for matters of this kind.
Of the women we spoke to, 77% said that they were either currently going through the menopause or had already experienced it. 63% said that their working life had been negatively affected in some way by their symptoms. 73% of women reported having hot flushes, while 63% said they regularly felt tired or drowsy. 48% suffered with low mood, 47% struggled to concentrate and 43% had trouble with their memory. As a result of this, 34% of women said that they had developed depression and anxiety, while 29% had significantly lost self confidence. Only 6% of the whole sample group said that they did not experience any menopause symptoms at work.
58% of the women surveyed by Forth said that they were still affected by symptoms of the menopause, and that this sometimes caused them problems at work. 41% said that their poor concentration or forgetfulness has led them to make more mistakes, while 40% admitted to losing interest in their job as a result. 11% forwent the opportunity for promotion because of the menopause, and 8% believed that their symptoms played some part in them resigning their position.
Our study showed that 24% of respondents had called in sick as a result of the menopause and almost half of those individuals said they’d done so more than once. A staggering 90% of the women who responded to our survey said that their workplace had no help available at all when it came to employees going through the menopause. 72% - just under three quarters - of the women who responded to Forth’s survey said that their workplace needed to improve the level of support that was available for individuals experiencing symptoms of the menopause.
Not all women want treatment to relieve symptoms of the menopause, but treatments are available if you find the symptoms particularly troublesome. The main treatment for menopausal symptoms is hormone replacement therapy (HRT), although other treatments are also available for some of the symptoms.
Hormone replacement therapy (HRT)
HRT involves taking oestrogen to replace the decline in your body's own levels around the time of the menopause. This can relieve many of the associated symptoms. National Institute for Health and Care Excellence (NICE) guidelines state that HRT is effective and should be offered to women with menopausal symptoms, after discussing the risks and benefits.
There are two main types of HRT:
- Combined HRT (oestrogen and progestogen) – for women with menopausal symptoms who still have their womb (oestrogen taken on its own can otherwise increase your risk of womb cancer)
- Oestrogen-only HRT – for women who have had their womb removed in a hysterectomy
HRT is available as tablets, skin patches, a gel to rub into the skin or implants. HRT is extremely effective at relieving menopausal symptoms, especially hot flushes and night sweats, but there are a number of side effects, including breast tenderness, headaches and vaginal bleeding. It's also associated with an increased risk of blood clots and breast cancer in some women. HRT is not advisable for some women, such as those who have had certain types of breast cancer or are at high risk of getting breast cancer. Your GP can give you more information about the risks and benefits of HRT to help you decide whether or not you want to take it.

In England, women are more likely than men to have a common mental health problem and are almost twice as likely to be diagnosed with anxiety disorders. 10% of mothers and 6% of fathers in the UK have mental health problems at any given time. More women than men experience depression. One in four women will require treatment for depression at some time, compared with one in 10 men. Many more girls than boys self-harm. Research suggests that between one in 12 and one in 15 young people self-harm in the UK.
Eating disorders are more common in women than men, with young women most likely to develop one. 1.9% of women and 0.2% of men experience anorexia in any year. Between 0.5% and 1% of young women experience bulimia at any one time. Women are twice as likely to experience anxiety disorders as men. About 60% of the people with phobias or obsessive compulsive disorder are women. Phobias affect about 22 in 1,000 women in the UK, compared with 13 in 1,000 men. Worldwide, more women are affected by PTSD than men, largely because women are exposed to more sexual violence. The risk of developing PTSD after any traumatic event is 20.4% for women and 8.1% for men. There are a range of factors as to why common mental health problems are more prevalent amongst women.
Women's increased life expectancy means they are more likely than men to outlive their partner and move into residential care. This means they are more at risk of depression associated with psycho-social factors. Most carers are women, whether they care for their children, partner, parents, other relatives or friends. Women carers are more likely to suffer from anxiety or depression than women in the general population. Three quarters of people who care for a person with a mental health problem are women and the average age of carers is 62 years.
Women in 'mid-life', aged 45-60 years, may be juggling caring commitments for children and older relatives as well as doing paid work and facing physical health problems. At the same time, mid-life women may find themselves in financial difficulty as a result of lifelong lower pay, part-time working, family caring, widowhood or divorce. This combination can increase their risk of experiencing mental distress.
The social factors particularly affecting women's mental health include:
More women than men are the main carer for their children and they may care for other dependent relatives too - intensive caring can affect emotional health, physical health, social activities and finances. Women often juggle multiple roles - they may be mothers, partners and carers as well as doing paid work and running a household. Women are overrepresented in low income, low status jobs - often part-time - and are more likely to live in poverty than men. Poverty, working mainly in the home on housework and concerns about personal safety can make women particularly isolated. Physical and sexual abuse of girls and women can have a long-term impact on their mental health, especially if no support has been received around past abuses.
Mental health problems affecting more women than men:
Although women are more likely to be affected by mental health disorders, they are also more likely to seek support. Women are more likely to have been treated for a mental health problem than men (29% compared with 17%). This reflects women's greater willingness to acknowledge that they are troubled and get support.
About 25% of people who die by suicide are women. Again, women's greater emotional literacy and readiness to talk to others about their feelings and seek help may protect them from suicidal feelings. Being a mother also makes women less likely to take their own life. Women's friendships with other women help protect their mental health, providing a source of support, particularly in hard times or at times of loss or change. Mentally healthy women generally talk about their feelings more than men and more often have stronger social networks of friends and family. They are more likely to tell someone when they are troubled, whether it is someone they are close to or someone who can offer medical advice. Good social support can play a part in preventing mental ill health and can help people recover from mental health problems.

Women can receive support from all of the same avenues men can but here are some specialist charities which can help:
Refuge:
Advice on dealing with domestic violence:
Phone: 0808 2000 247 (24-hour helpline)
Website: www.refuge.org.uk
NSPCC:
If you are concerned for the safety of your children or someone elses:
Children's charity dedicated to ending child abuse and child cruelty.
Phone: 0800 1111 for Childline for children (24-hour helpline)
0808 800 5000 for adults concerned about a child (24-hour helpline)
Website: www.nspcc.org.uk
Rape Crisis:
To find your local services phone: 0808 802 9999 (daily, 12pm to 2.30pm and 7pm to 9.30pm)
Website: www.rapecrisis.org.uk
Beat:
If you are living with an eating disorder:
Phone: 0808 801 0677 (adults) or 0808 801 0711 (for under-18s)
Website: www.b-eat.co.uk